On This Page
Dhamasa – The Potential Plant that Thrive in Extremely Arid Regions
Introduction
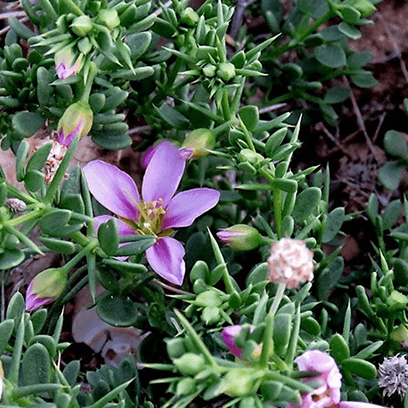
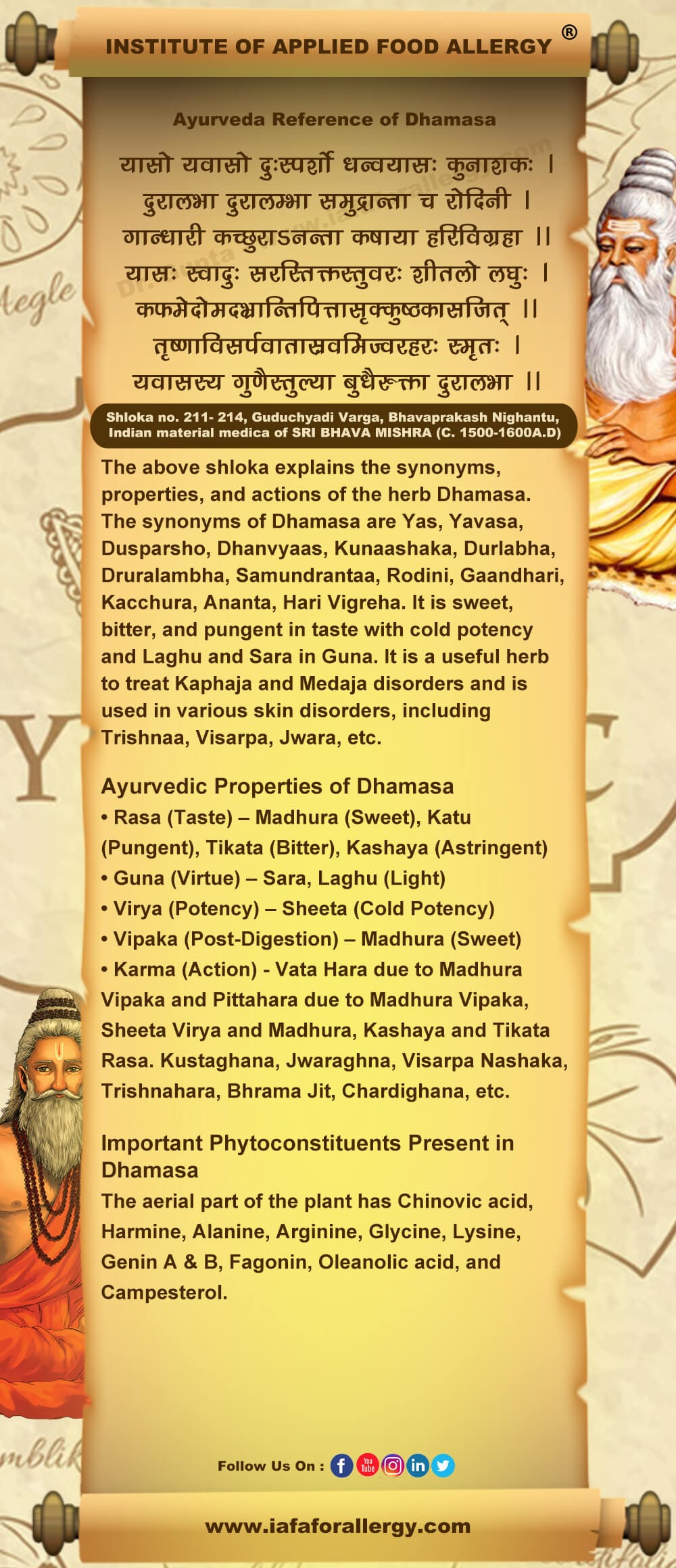
Dhamasa or Fagonia cretica, famous with the name Virgin’s mantle, is a hardy shrub which is highly valued for its medicinal properties. Dhamasa is known for its ability to thrive in extremely arid and semi-arid regions, often growing in rocky and dessert – like terrains where few other plants can survive. Dhamasa is commonly found in arid and semi-arid regions and widely distributed in the Indian subcontinent particularly in Punjab, Gujrat and Rajasthan. Dhamasa is mainly used for treatment of fever, UTI, liver condition, etc. In Ayurvedic classical literature Dhamasa is mentioned as Madhura (sweet), Tikata (bitter), and Katu (pungent) in taste with cold potency (Sheeta Virya) and Laghu and Sara in Guna. It is a useful herb to treat Kaphaja and Medaja disorders and is used in various skin disorders, including Trishnaa, Visarpa, Jwara, etc. Recent research revealed that Dhamasa consist of Chinovic acid, Harmine, Alanine, Arginine, Glycine, Lysine, Genin A & B, Fagonin, Oleanolic acid, etc due to which it exhibits antioxidant, anti-tumor, cardioprotective, anti-diabetic activities, etc.
Basonym of Drug
धन्वन: यास: मरुदेशे जायमान त्वात |
Dhanvayasa / Dhamasa grows in dry lands or regions.
Synonyms
- According to Habitat
मरू उद्भव: – मरू देशे जात: |
Dhamasa grows in dry regions.
गान्धारी- गांधार देशे बाहुल्येनोपलब्धा |
Dhanvayasa is very common in Gnadhara Desha i.e. Afghanistan.
- According to Morphology
अनंता – न अनन्तो अस्या: विस्तृत त्वात |
Dhanvayasa spreads extensively on the ground.
ताम्रमूली – ताम्र वर्ण मूलमस्य |
The root of Dhamasa is coppery in color.
दुरालभा – दुःखेन लभ्यते दूरवर्ती त्वात कंटकित्वाच |
Dhamasa has thorns, so they are difficult to hold.
अग्रहा- ग्रहीतुम शक्या कंटकि त्वात |
Dhamasa is a difficult plant to hold because of thorns.
- According to Properties and Action
कषाया- स्वादे कषाया प्राया |
Dhamasa has astringent taste
Regional Names of Dhamasa (Fagonia cretica)
- Khorasan thorn, Camel thorn, Persian Manna plant (English)
- Usturgar, Javasa, Dhanhare, Hinguaa (Hindi)
- Dhamaaso (Gujarati)
- Dhamasa (Marathi)
- Dusparsha (Kannada)
- Kodittuva (Malayalam)
- Tulganaari (Tamil)
- Chittigava, Gilaregati (Telugu)
- Dama, Damaha (Punjabi)
Botanical Name
Fagonia cretica Linn.
Fagonia word is derived from a Physician of France Monsignor Fagon and cretica means inhabiting in chalky soils.
Family – Zygophyllaceae (Goksura Kula)
Ayurveda Reference for Dhamasa (Fagonia cretica)
Scientific Classification of Dhamasa (Fagonia cretica)
| Kingdom | Plantae |
| Sub-Kingdom | Viridaeplantae |
| Class | Magnoliopsida |
| Order | Zygophyllales |
| Family | Zygophyllaceae |
| Genus | Fagonia |
| Species | Cretica |
Classification of Dhamasa’s – As Per Charaka and Sushruta
Charaka: Trishna Nigrehana Mahakshaya, Arshoghana Mahakshaya.
Sushruta: Guduchyadi Gana.
Dhamasa’s Description in Brihtrayi as Duhsparsha, Dushsparsha, Dushsparshaka
| Charaka | Shusruta | Vagbhata (Ashtang Hridya) |
| C. S. Chi. 14/ 100, 197 | S. S. Chi. 11/ 8 | A. H. Chi. 1/ 45 |
| C. S. Chi. 15/ 187 | S. S. U. 55/ 25 | A. H. Chi. 3/ 14, 160 |
| C. S. Chi. 18/ 51, 159 | A. H. Chi. 7/ 34 | |
| C. S. Chi. 24/ 166 | A. H. Chi. 8/ 63 |
Dhamasa’s Description in Brihtrayi as Duralabha / Duralambha
| Charaka | Shusruta | Vagbhata (Ashtang Hridya) |
| C. S. Su. 4/ 30, 36 | S. S. Su. 44/ 26 | A. H. Sa. 2/ 8 |
| C. S. Su. 25/ 39 | S. S. Chi. 9/ 8, 9 | A. H. Chi. 1/ 51, 54 |
| C. S. Chi. 3/ 198, 211, 213, 225 | S. S. U. 39/ 188, 243, 246 | A. H. Chi. 2/ 17 |
| C. S. Chi. 4/ 75 | S. S. U. 40/ 63 | A. H. Chi. 3/ 13, 39, 49, 61 |
| C. S. Chi. 5/ 119 | S. S. U. 51/ 32, 39 | A. H. Chi. 4/ 21 |
| C. S. Chi. 7/ 103, 140 | S. S. U. 52/ 30 | A. H. Chi. 5/ 17 |
| C. S. Chi. 8/ 100, 106, 112, 126 | A. H. Chi. 6/ 21 | |
| C. S. Chi. 10/ 19 | A. H. Chi. 7/ 106 | |
| C. S. Chi. 14/ 154 | A. H. Chi. 8/ 70, 149 | |
| C. S. Chi. 15/ 134, 153, 180 | A. H. Chi. 9/ 62 | |
| C. S. Chi. 16/ 47 | A. H. Chi. 18/ 6 | |
| C. S. Chi. 17/ 94 | A. H. Chi. 19/ 2 | |
| C. S. Chi. 18/ 50, 53, 63, 118, 127 | A. H. Ka. 2/ 25, 29 | |
| C. S. Chi. 19/ 58, 60 | A. H. U. 7/ 20 | |
| C. S. Chi. 20/ 38 | ||
| C. S. Chi. 21/ 54 | ||
| C. S. Ka. 7/ 50, 55, 59 |
Durva’s Description in Brihtrayi as Yavasa, Yavasaka
Yavasa is botanically Alhagi pseudolhagi. Both have similar properties so can be used in each other’s place.
Charaka Samhita: C. S. Su. 3/ 26, C. S. Chi. 3/ 222, C. S. Chi. 4/ 68, 75, 100, 103, C. S. Chi. 14/ 215, 226, C. S. Chi. 26/ 209
Sushruta Samhita: S. S. Su. 44/ 49, S. S. Su. 45/ 167, S. S. Su. 39/ 217- 220, S. S. Su. 52/ 42
Vagbhatta: A. H. Chi. 8/ 125, A. H. U. 22/ 92, 97
Durva’s Description in Brihtrayi as Dhanyavyasa (Controversy)
Although Dhamasa and Yavasa are identified with Fagonia cretica Linn, and Alhagi pseudalhagi (Bieb.) Dev. respectively and they belong to different families, they are almost identical in their properties and have been used as substitutes (Vide A. H. U. 13.7 and S. S. U. 39. 222 in identical Yoga). Both these two plants are also similar in their habit and habitat. Duralabha seems to be used as a synonym for Dhanvayasa in A. H. (Vide Chi. 3. 64; 13. 14 and 19. 10) and C. S. (Vide Ci. 18. 52; 5. 118 and 7. 139). Both the names Duhsparsa and Dunsparsaka have also been accepted as synonyms of Dhanvayasa. Duhsparsa again is a synonym of Kantakari and Kapikacchu. Lastly, Ananta-Amaar has usually been accepted as another name for Sariva- Antana but some commentators in some places have taken it to be equivalent to Dhanvayasa and Durva as well.
Charaka Samhita: C. S. Su. 4/ 12, 29, C. S. Chi. 3/ 204, 208, C. S. Chi. 4/ 45, C. S. Chi. 7/ 145, C. S. Chi. 14/ 187, C. S. Chi. 18/ 178, C. S. Chi. 21/ 57, C. S. Chi. 26/ 170
Vagbhata: A. H. Su. 10/ 29, A. H. Chi. 1/ 53, 65, 69, A. H. Chi. 3/ 64, A. H. Chi. 8/ 102, A. H. Chi. 11/ 37, A. H. Chi. 13/ 14, A. H. Chi. 14/ 49, A. H. Chi. 19/ 10, A. H. U. 13/ 7, A. H. U. 24/ 54, A. H. U. 30/ 12
Durva’s Description in Brihtrayi as Ananta (Controversy)
It has been identified with any one of these, Sariva, Dhanvaysa, and Durva. In many places, it has been used with Sariva, and in some, it has been used with Durva or Yasa. As each of these three has two varieties, Ananta may indicate the use of the second variety in such cases. As all three appear to have partial similarity in their effects, any of these may also be used. The name Ananta probably refers to the indefinite growth of the whole plant (in the case of Durva) or a part of it (primary root only in the case of Dhanvayusa). The long traditional use of Sariva under the name of Anantamula may indicate Vaidyas’ preference for Sariva.
| Charaka | Shusruta | Vagbhata (Ashtang Hridya) |
| C. S. Su. 4/ 31 | S. S. Su. 16/ 20. 27 | A. H. Su. 15/ 6, 37 |
| C. S. Su. 25/ 39 | S. S. Su. 36/ 7 | A. H. Sa. 2/ 55, 59 |
| C. S. Vi. 8/ 151 | S. S. Chi. 3/ 61 | A. H. Chi. 8/ 113 |
| C. S. Sa. 8/ 41 | S. S. Chi. 11/ 9 | A. H. Chi. 18/ 15 |
| C. S. Chi. 3/ 257 | S. S. Chi. 38/ 54 | A. H. Ka. 4/ 12 |
| C. S. Chi. 4/ 102 | S. S. Ka. 3/ 12 | A. H. U. 1/ 13 |
| C. S. Chi. 9/ 41 | S. S. Ka. 6/ 3 | A. H. U. 3/ 49 |
| C. S. Chi. 21/ 87 | S. S. Sa. 10/ 60, 64 | A. H. U. 6/ 39 |
| C. S. Chi. 23/ 231 | S. S. U. 10/ 5 | A. H. U. 13/ 76, 93 |
| C. S. Chi. 26/ 178, 232 | S. S. U. 24/ 40 | A. H. U. 18/ 8 |
| C. S. Chi. 30/ 91 | S. S. U. 29/ 7 | A. H. U. 22/ 36, 88 |
| C. S. Si. 3/ 46 | S. S. U. 33/ 7 | A. H. U. 34/ 47 |
| C. S. Si. 20/ 41 | S. S. U. 36/ 4 | |
| S. S. U. 39/ 204 | ||
| S. S. U. 62/ 31 |
Controversy of Dhamasa / Dhanvyasa with Yavasa
In Rigveda, a herb named ‘Yavasa’ is described as fodder for cattle (R.V. 1/ 38/ 5, 1/ 91/ 13; 7/ 18/ 10). Another herb ‘Yavasa’ is also found in Vedic literature. However, it is not confirmed whether these two are the same as the Yavasa of Samhitas. Charaka as well as Sushruta have mentioned Yavasa and Yasa Sarkara in their texts. Dalhana explained the water extract of Yavasa as Yasa Sarkara. It is generally accepted that Yavasa and Duralabha are synonymous. Thakurji described that both have similar properties and may be used in each other’s place.
Bhavamisra explained both these herbs separately, but their properties are mentioned as similar. The origin of this controversy may be because of Adhamalla’s view wherein he considered Yavasaka as the substitute for Duralabha. At present A. camelorum and Fagonia arabica / cretica Linn are considered as Yavasa and Duralabha respectively.
Different Varieties – Yasa and Dhanvayasa are considered as two varieties in Sodhala Nighantu.
External Morphology of Fagonia cretica
- Habit: Dhamasa is a small erect undershrub, spinous. The branches are slender and glabrous.
- Leaves: Leaves of Dhamasa are opposite, 1 to trifoliate. Petioles are variable in length up to 3 cm long, 2 pairs of thorny stipules sometimes 1 cm long. Leaflets of Dhamasa are linear, acute, sessile, or with very short petiolules.
- Flowers: Flowers of Dhamasa are small, light pink.
- Fruits: Fruits of Dhamasa are glandular, pubescent, rounded at the base, and pyramidal towards the apex.
- Seeds: Seeds of Dhamasa are ovoid, acute, and smooth with flattened surfaces.
Flowering and fruiting time
Flowering occurs in April, May, and June.
Distribution of Dhamasa
Dhamasa is found throughout the desert region of Western India and Pakistan. It is also found in Cyprus, North Africa, Spain, Turkey, etc.
The Useful Part of Dhamasa
Panchanga (Whole plant)
Varieties of Dhamasa
Raja Nighantu mentioned two varieties of Dhamasa:
- Duralabha
- Kshudra Duralabha
Important Phytoconstituents of Dhamasa
The aerial part of the plant has Chinovic acid, Harmine, Alanine, Arginine, Glycine, Lysine, Genin A & B, Fagonin, Oleanolic acid, and Campesterol.
Recent Research on Dhamasa (Fagonia cretica)
- Qureshi, Huma & Asif, Saira & Ahmed, Haroon & Al-Kahtani, Hassan & Hayat, Khizar. (2016). Chemical composition and medicinal significance of Fagonia cretica: A review. Natural product research. 30. 625- 639. 10. 1080/ 14786419. 2015. 1036268.
- Puri, Dinesh & Anil, Bhandari. (2015). Fagonia: A potential medicinal desert plant. Journal of Nepal Pharmaceutical Association. 27. 10. 3126/ jnpa. v27i1. 12147.
- Hussain, A. & Zia, Muhammad & Mirza, Bushra. (2007). Cytotoxic and antitumor potential of Fagonia cretica L. Turkish Journal of Biology. 31. 19- 24. According to traditional knowledge, Fagonia cretica has medicinal potential, especially against cancer and tumors. In the present study, this information was analyzed at the laboratory level by performing cytotoxic, antitumor (potato disc), and DNA damage assays. Significant cytotoxic activity was found against brine shrimps at LD50 118. 89 ppm, while the antitumor assay showed that the extract inhibited tumor induction on potato discs. Significant antitumor activity was found against all the tumor-inducing Agrobacterium strains tested (At6, At10, and At77), with maximum tumor inhibition (77.04%) against At10. However, the extract did not show any lethal activity against Agrobacterium tumefaciens strains, and no DNA-damaging activity was observed. The overall results indicate a strong anti-cancerous potential of this plant.
- Sajid, B. & Erum, Alia & Rizwana, K. & Uzma, Saeed, Alamgeer. (2011). Phytochemical screening and antimicrobial activity of Fagonia cretica plant extracts against selected microbes. J Pharm Res. 4. 962- 963.
- Saleem, Uzma. (2011). Phytochemical screening and antimicrobial activity of Fagonia cretica plant extracts against selected microbes. Journal of Pharmacy Research. 4. 962- 963. Fagonia cretica L is a small spiny shrub mostly located in dry rocky areas of Pakistan. It is well-known in scientific and folkloric literature due to its medicinal uses. In the present study, the active phytocomponents of Fagonia cretica were revealed using phytochemical analysis. Antimicrobial activity of Fagonia cretica plant extracts (aqueous, methanolic, ethanolic) of different concentrations were tested against S.aureus, B.subtilis S.epidermidis E.coli, and P.aeruginosa by disc diffusion method. MIC of plant extract was also carried out against S.aureus, P.aeruginosa, and B.subtilis. The preliminary phytochemical screening of the Fagonia cretica plant showed the presence of bioactive compounds. Aqueous and methanolic extracts showed more activity against all the tested bacteria as compared to ethanolic extract. The results scientifically validate the use of this plant in traditional medicines and the isolation and characterization of the active principle for further exploitation in medical microbiology.
- Saeed, M & Sabir, A. (2003). Effects of Fagonia cretica L constituents on various hematological parameters in rabbits. Journal of Ethnopharmacology. 85. 195- 200. 10. 1016/ S0378- 8741 (02) 00365- 3.
- Tabassum, Tanzila & Tawab, Abdul & Hameed, H & Alshiekheid, M & Alzahrani, Khalid & Banjer, Hamsa & Rahman, Hazir. (2022). Fagonia cretica: Identification of compounds in bioactive gradient high-performance liquid chromatography fractions against multidrug-resistant human gut pathogens. Tropical Biomedicine. 39. 185- 190. 10. 47665/ tb. 39. 2. 006. Plants are an alternative source of natural medicines due to secondary active metabolites. Fagonia cretica extracts and Gradient High-Pressure Liquid Chromatography fractionations were checked against multidrug-resistant gastrointestinal pathogens including Salmonella typhi, Escherichia coli, and Shigella flexneri. ESI-MS/MS analysis of bioactive HPLC fractions was performed to elucidate antibacterial compounds. F. cretica extracts exhibited potential antibacterial activity. Twenty-four (24) HPLC fractions were obtained from methanol, ethanol, and aqueous extracts of F. cretica. Eighteen (18) fractions showed antibacterial activity, while no activity was observed by the remaining six (6) fractions. HPLC fractions, F1 (25 g ± 0.20 mm) and F2 (15 f ± 0.12 mm) of aqueous extract exhibited activity against multidrug-resistant GI pathogens. Gallic acid, quinic acid, cyclo-l-leu-l-pro, vidalenolone, liquirtigenin, rosmarinic acid, and cerebronic acid were identified in F1 fraction of aqueous extract, while succinic acid, cyclo (l- Leu- l- Pro) and liquirtigenin were identified in F2 fraction of aqueous extract through ESI-MS/MS analysis. F. cretica extracts and HPLC fractions showed potential activity against MDR GI pathogens. Vidalenolone, Cyclo- 1- leu- 1- pro and Cerebronic acid are first time reported in F. cretica. Further characterization of bioactive compounds from F. cretica may help elucidate antibacterial therapeutic molecules.
- Tunio, Qamar- U- Nisa & Rafiq, Muhammad & Tunio, Azhar & Qureshi, Abdul & Charan, Tanzeel & Bhutto, Mihr & LASHARI, Zubeda. (2022). Determination of Phytochemicals, Antimicrobial, Antioxidant and Allelopathic Effects of Fagonia cretica L. Yuzuncu Yıl Universitesi Tarım Bilimleri Dergisi. 32. 785- 794. 10. 29133/ yyutbd. 1122798. The medicinal plant Fagonia cretica L., is well known in traditional medicines for curing various complaints of human beings from ancient times and is locally known as Dhamasa. Previous studies have reported the presence of many phytochemicals, antimicrobial, and antioxidant properties in the various parts of this plant. Therefore, here in this study, we have presented a comprehensive study on the presence of similar medicinal and chemical properties of Dhamsa found in Jamshoro District, Pakistan. For this study, extracts of the root, stem, leaf, and pod of the plant were prepared separately from three different solvents, water, ethanol, and methanol. Then the amount and presence of various phytochemicals, antimicrobial, antioxidant properties, and allelopathic effects were determined in all the extracts. The obtained results of this study confirm the presence of medicinal important phytochemicals in the plant extracts. The antimicrobial testing of this plant proved its highest activity against E. coli (16 ± 1.4mm), Salmonella typhi (18± 0.7 mm), and Pseudomonas aeruginosa (15± 1.4 mm) in methanol, water, and ethanol extracts respectively. The presence of antioxidant activities was also observed in the ethanolic extract of the leaf at about 0.98 mg/ ml. This plant showed allelopathic effects on the growth of radish and spinach plants. So, we have concluded this study that Fagonia cretica L., collected from Jamshoro has the same or more important properties compared to the same plant from other regions, which proves the similar significant value of the Fagonia cretica plant of Jamshoro in various fields of medicinal sciences.
- Satpute, Ravindra & Bhattacharya, Rahul & Kashyap, Rajpal & Purohit, Hemant & Deopujari, Jayant & Taori, Girdhar & Daginawala, Hatim. (2012). Antioxidant Potential of Fagonia arabica against the Chemical Ischemia-Induced in PC12 Cells. Iranian journal of pharmaceutical research: IJPR. 11. 303- 13. The imbalance between pro-oxidants and antioxidants leads to the generation of oxygen/nitrogen free radicals which are implicated in several neurodegenerative diseases. Fagonia arabica is an ethno-pharmacologically important Ayurvedic herb known to have many medicinal properties like anti-inflammatory, analgesic, and antipyretic effects. However, its antioxidant potential has not been investigated so far. The present study was designed to investigate the antioxidant potential of F. arabica and its neuroprotective effect on chemical ischemia induced in PC12 cells. Chemical ischemia was induced by exposing the cells to an uncoupler of oxidative phosphorylation sodium azide (5.0 mM) and competitive inhibitor of glycolysis 2- deoxyglucose (2.0 mM) for 2 h followed by 24 h reperfusion with normal culture medium. The total polyphenolic content (TPC) and antioxidant potential of the herb were measured using DPPH and ABTS•+ scavenging and ferric ion reducing antioxidant potential (FRAP) assays; its effect on neuroprotection and energy metabolism was also studied. The ischemic injury was characterized by impaired energy status as indicated by decreased ATP levels in the cells, accompanied by increased lactic acid content. Both the changes favourably responded to F. arabica offered considerable neuroprotection from ischemia and helped to maintain the cellular viability and mitochondrial integrity of the cells. F. arabica showed a considerable amount of TPC and antioxidant activity. This study reveals the antioxidant potential of F. arabica and its protective efficacy against ischemia/reperfusion-mediated cell death. F. arabica thus can be considered for further studies for the development of the prophylactic or therapeutic agent for the treatment of ischemic stroke.
- Anjum, Muhammad & Ahmed, Ejaz & Jabbar, Abdul & Malik, Azad & Ashraf, Mujeeb & Moazzam, Muhammad & Rasool, Azam. (2007). Antimicrobial Constituents from Fagonia cretica. Journal of the Chemical Society of Pakistan. 29. 634-639. Eleven compounds have been isolated for the first time from the whole plant of Fagonia cretica and their structures are elucidated by extensive spectroscopic studies. All the isolated compounds are tested for their antimicrobial activity.
- Khalid, Samrah & Tiwana, Hira & Saddiqi, Fatima & Ali, Khaver & Adil, Muhammad & Javed, Tariq & Riaz, Sana. (2021). In vitro antimutagenic, cytotoxic, and anticancer potential of Fagonia indica phytochemicals. Pakistan journal of pharmaceutical sciences. 34. 2325- 2331. Cancer is one of the most diagnosed and life-threatening diseases throughout the world. Nevertheless, present-day clinical management for cancers is surgery, radiations which are insufficient to contain the disease burden. In the past two decades, more than half of chemotherapeutic drugs developed are either directly or indirectly dependent on medicinal base phytocompounds or their derivatives. The present study aims to provide the base for chemotherapeutic phytochemicals. Fagonia indica showed significant antimutagenic potential concerning control IC50 values were calculated as 146.33± 5.2 μg/ ml, TA100 (AZS) 105.33± 4.0 μg/ ml, TA98 (2AA) 113.6± 5.2 μg/ ml followed and TA98 (AZS) 112.6± 4.4 in Ame’s test. For this reason, the antiproliferation effect of extracts on cancer cell lines was studied through resazurin fluorescence. On HepG-2 cell lines, 50% cytotoxic concentration (CC50) of (FIWM) was recorded as 128.3±,2.43μg/ml. On the homo sapiens epithelial cell of lung tissue (A549), the high throughput instrumental analysis of Fagonia indica depicts maximum cytotoxic effect in 30hr. The electrical impedance displays the real-time evidence of qualitative apoptosis expressed. The impedance results were supported as palmitic acid from Fagonia indica virtually inhibits Cyclin Dependent Kinase 2 (CDKs 2) in silico molecular docking studies. Fagonia indica extract possesses substantial antimutagenic, cytotoxic, and anticancer activity which supports the potential of its phytochemicals for drug development.
- Lam, Matt & Carmichael, Amtul & Griffiths, Helen. (2012). An Aqueous Extract of Fagonia cretica Induces DNA Damage, Cell Cycle Arrest, and Apoptosis in Breast Cancer Cells via FOXO3a and p53 Expression. PloS one. 7. e40152. 10. 1371/ journal. phone. 0040152. Plants have proved to be an important source of anti-cancer drugs. Here we have investigated the cytotoxic action of an aqueous extract of Fagonia cretica, used widely as a herbal tea-based treatment for breast cancer.
- Khan, Haider Ali & Ghufran, Mehreen & Shams, Sulaiman & Jamal, Alam & Ayaz, Muhammad & Ullah, Mehran & Khan, Abbas & Khan, Mohammad Imran & Awan, Zuhier. (2023). In-depth in-vitro and in-vivo anti-diabetic evaluations of Fagonia cretica mediated biosynthesized selenium nanoparticles. Biomedicine & pharmacotherapy Biomedicine & pharmacotherapy. 164. 10. 1016/ j. biopha. 2023. 114872. Therapeutic moieties derived from medicinal plants as well as plant-based ecofriendly processes for producing selenium nanoparticles have shown great promise in the management of type 2 diabetes mellitus (T2DM). The current study aimed to assess the anti-diabetic potentials of Fagonia cretica-mediated biogenic selenium nanoparticles (FcSeNPs) using in-vitro and in-vivo approaches. The bio-synthesized FcSeNPs were characterized using various techniques including UV- VIS spectrophotometry and FTIR analysis. The in-vitro efficacy of FcSeNPs was assessed against α-glucosidase, and α-amylase enzymes as well, and the anti-radical studies were performed using DPPH and ABTS free radicals scavenging assays. For in-vivo studies, 20 Male Balb/C albino-mice were randomly divided into 4 groups (n = 5) including a normal group, a disease group (Diabetic group with no treatment), a control group, and a treatment group (Diabetic group treated with FcSeNPs). Further, biochemistry markers including pancreas, liver, kidney, and lipid profile were assessed for all treatment groups. The FcSeNPs exhibited a dose-dependent inhibition against α-amylase and α-glucosidase at 62-1000 µg mL-1 concentration with IC50 values of 92 and 100 µg mL-1 respectively. In antioxidant experiments, the FcSeNPs demonstrated significant radical scavenging effects against DPPH and ABTS radicals. In STZ-induced diabetic mice, a considerable decline in blood glucose levels was observed after treatment with FcSeNPs. Anti-hyperglycemic effect of FcSeNPs treated animals was high (105 ± 3.22) as compared to the standard drug (128.6 ± 2.73 mg dL- 1). Biochemical investigations revealed that all biochemical parameters for the pancreas, liver function, renal function panel, and lipid profile were significantly lowered in FcSeNPs-treated animals. Our findings indicate a preliminary multi-target efficacy for FcSeNPs against type-2 diabetes and thus warrant further detailed studies.
- Using flow cytometric analysis of cells labeled with cyclin A, annexin V, and propidium iodide, we describe a time and dose-dependent arrest of the cell cycle in the G0/ G1 phase of the cell cycle and apoptosis following extract treatment in MCF-7 (WT- p53) and MDA- MB- 231 (mutant- p53) human breast cancer cell lines with a markedly reduced effect on primary human mammary epithelial cells. Analysis of p53 protein expression and its downstream transcription targets, p21, and BAX, revealed a p53-associated growth arrest within 5 hours of extract treatment and apoptosis within 24 hours. DNA double-strand breaks measured as γ- H2AX were detected early in both MCF-7 and MDA-MB-231 cells. However, loss of cell viability was only partly due to a p53-driven response as MDA- MB-2 31 and p53-knockdown MCF- 7 cells both underwent cell cycle arrest and death following extract treatment. p53- independent growth arrest and cytotoxicity following DNA damage have been previously ascribed to FOXO3a expression. Here, in MCF-7 and MDA- MB- 231 cells, FOXO3a expression was increased significantly within 3 hours of extract treatment and FOXO3 siRNA reduced the extract-induced loss of cell viability in both cell lines. Our results demonstrate for the first time that an aqueous extract of Fagonia cretica can induce cell cycle arrest and apoptosis via p53-dependent and independent mechanisms, with activation of the DNA damage response. We also show that FOXO3a is required for activity in the absence of p53. Our findings indicate that Fagonia cretica aqueous extract contains potential anti-cancer agents acting either singly or in combination against breast cancer cell proliferation via DNA damage-induced FOXO3a and p53 expression.
- Kamran, Sairah & Shoaib, Rana & Ahmad, Mariya & Ishtiaq, Saiqa & Anwar, Rukhsana. (2017). Antidiabetic and reno-protective effect of Fagonia cretica L. methanolic extract and Citrus paradise Macfad. juice in alloxan-induced diabetic rabbits. Journal of Pharmacy and Pharmacognosy Research. 5. 345- 353. 10. 56499/ jppres- 17. 230_5. 6. 365. Context: Fagonia cretica is a medicinal herb reported to have flavanoids of potential therapeutic value and Citrus paradisi is a fruit, whose juice is of great therapeutic value due to its anti-hyperglycemic effects. Aims: To determine the anti-hyperglycemic and renal protective effect of methanolic extract of Fagonia cretica and Citrus paradisi juice (grapefruit juice) in alloxan-induced diabetic rabbits. Methods: Diabetes was induced in rabbits by alloxan monohydrate (150 mg/ kg, i.p.). The therapies including Fagonia cretica methanolic extract (500 mg/ kg), Citrus paradisi juice (7 mL/ kg), and sitagliptin (10 mg/ kg) were administered (p. o.) to diabetic groups for 14 days. The biochemical parameters, glucose, creatinine, urea, bilirubin, albumin, total protein, globulins, and albumin/globulin ratio were estimated. Results: Fagonia cretica extract and grapefruit juice therapy significantly (p< 0.05) reduced glucose levels in diabetic rats. Fagonia cretica extract was a more effective anti-hyperglycemic agent than Citrus paradisi juice and sitagliptin. Significant (p< 0.05) improvement in kidney function was observed in treated groups, with the plant extract showing significant improvement as compared to the other two treatments. The histopathological results verified improvement in structural damage of the kidney, liver, and pancreas with these treatments. Conclusions: Fagonica cretica and Citrus paradisi juice therapy markedly improved hyperglycemia and kidney functions in alloxan-induced diabetic rabbits.
- Al- Ziaydi, Ahmed. (2018). Protective effect of Fagonia arabica (L.) against Alloxan monohydrate-induced Diabetes in albino Wistar rat. Abstract Diabetes mellitus is a most common endocrine disorder, affecting more than
- 300 million people worldwide. For this, therapies developed along the principles of Western medicine (allopathic) are often limited in efficacy, carry the risk of adverse effects, and are often too costly. To identify complementary or alternative approaches to existing medications, we studied the anti-diabetic potential of Fagonia Ethanolic extract of the plant F. arabica (L.). We have selected (L.). arabica using the Soxhlet apparatus with 70% ethanol. This extract was used to treat prepared by Alloxan monohydrate, one of the chemicals the diabetic rats use through oral ingestion. agents used to induce diabetes mellitus in animals. It induces diabetes by dose-dependent destruction of β -cells of islets of Langerhans. Diabetes was induced by a single I.P. dose of Alloxan monohydrate (150 mg/kg body weight). It was observed that a single intravenous dose of alloxan exhibited significant hyperglycemia. The study was carried out on a 45-day protocol and the body weights, and blood glucose levels were measured on Day 1, Day 7, Day 14, Day 21, Day 28, Day 35, Day 42, and Day 45 of the treatment, along with assays of AST, ALT, ALP, Lipid profile studies and histopathological examination of liver on day 45. Maximum activity was shown by the active compound with a percent variation in blood glucose levels. Glibenclamide (10 mg/kg body weight) was taken as the standard and the results were quite comparable with it. Because of the antioxidant and hypolipidemic activity of F.arabica, we have selected to know the anti-diabetic properties of the plant. There is no information available on the anti-diabetic activity of F.arabica. Hence the present study is designed to evaluate the anti-diabetic properties of the F.arabica in Alloxan monohydrate induced diabetes in albino Wistar rats.
- Azam, Fareeha & Sheikh, N. & Ali, Gibran & Tayyeb, Asima. (2018). Fagonia indica Repairs Hepatic Damage through Expression Regulation of Toll-Like Receptors in a Liver Injury Model. Journal of Immunology Research. 2018. 1- 12. 10. 1155/ 2018/ 7967135. Fagonia indica is a traditionally used phytomedicine to cure hepatic ailments. However, efficient validation of its hepatoprotective effect and the molecular mechanisms involved are not yet well established. Therefore, the present study was designed to evaluate the hepatoprotective activity of Fagonia indica and to understand the molecular mechanisms involved in the reversal of hepatic injury. The liver injury mouse model was established by thioacetamide followed by oral administration of plant extract. Serum biochemical and histological analyses were performed to assess the level of hepatic injury. Expression analysis of proinflammatory, hepatic, and immune regulatory genes was performed with RT- PCR. Results of serological and histological analyses described the restoration of normal liver function and architecture in mice treated with plant extract. In addition, altered expression of proinflammatory (IL- 1 β, IL-6, TNF- α, and TGF- β) and hepatic (krt-18 and albumin) markers further strengthen the liver injury reversal effects of Fagonia indica. Furthermore, a significant expression regulation of innate immunity components such as toll-like receptors 4 and 9 and MyD- 88 was observed suggesting an immune regulatory role of the plant in curing liver injury. In conclusion, the current study not only proposes Fagonia indica, a strong hepatoprotective candidate but also recommends an immune regulatory toll-like receptor pathway as an important therapeutic target in liver diseases.
- Pareek, Anil & Godavarthi, Ashok & Issarani, Roshan & Nagori, Badri. (2013). Antioxidant and hepatoprotective activity of Fagonia schweinfurthii (Hadidi) Hadidi extract in carbon tetrachloride-induced hepatotoxicity in HepG2 cell line and rats. Journal of Ethnopharmacology. 150. 10. 1016/ j. jep. 2013. 09. 048. The whole plant of Fagonia schweinfurthii (Hadidi) Hadidi (Family: Zygophyllaceae) is used in a variety of diseases including hepatic ailments in deserts and dry areas of India. To evaluate the antioxidant and hepatoprotective activity of ethanolic extract from Fagonia schweinfurthii (Hadidi) Hadidi (FSEE) in carbon tetrachloride (CCl4) induced hepatotoxicity in HepG2 cell line and rats. In vitro, antioxidant activity was determined by DPPH, ABTS radicals, and hydrogen peroxide methods. In vitro, cytotoxicity and hepatoprotective potential of FSEE were evaluated using HepG2 cells. Based on the cytotoxicity assay, FSEE (50, 100, 200 µg/ ml) was assessed for hepatoprotective potential against CCl4-induced toxicity in HepG2 cell line by monitoring cell viability, aspartate aminotransferase (AST), alanine aminotransaminase (ALT), lactate dehydrogenase (LDH) leakage, lipid peroxidation (LPO) and glutathione level (GSH). Further, in vivo, hepatoprotective activity of FSEE was evaluated against CCl4-induced hepatotoxicity in male Wistar albino rats. Rats were pre-treated with FSEE (200mg, 400mgkg(-1) day(-1) p.o.) for 7 days followed by a single dose of CCl4 (1.0 ml/ kg, i.p.) on the 8th day. Silymarin was used as a positive control. After 24h of CCl4 administration, various biochemical parameters like aspartate aminotransferase (AST), alanine aminotransaminase (ALT), alkaline phosphatase (ALP), total bilirubin (TB) and total protein (TP) levels were estimated in serum. The antioxidant parameters like superoxide dismutase (SOD) activity, catalase (CAT) activity, glutathione (GSH) content, and malondialdehyde (MDA) level in the liver homogenate were determined. Histopathological changes in the liver of different groups were also studied. The FSEE possessed strong antioxidant activity in vitro. The results indicated that CCl4 treatment caused a significant decrease in cell viability. The CCl4-induced changes in the HepG2 cells were significantly ameliorated by treatment of the FSEE. FSEE significantly prevented CCl4-induced elevation of AST, ALT, ALP, TB, and CCl4-induced decrease in total protein in rats. FSEE-treated rat liver antioxidant parameters (SOD, CAT, MDA, and GSH,) were significantly antagonized for the pro-oxidant effect of CCl4. Histopathological studies also supported the protective effect of FSEE. The results of this study revealed that FSEE has significant hepatoprotective activity. This effect may be due to the ability of the extract to inhibit lipid peroxidation and increase the antioxidant enzymatic activity.
Recent Research on Alhagi pseudalhagi / Alhagi camelorum
- Aytaç, Ezgi & Laghari, Abdul & Sokmen, Munevver & Memon, Shahabuddin. (2014). Antioxidant Activity of Alhagi camelorum Phenolics Extracted by Automated and Standard Extraction Techniques. Separation of Science and Technology. 50. 529- 535. 10. 1080/ 01496395. 2014. 956763. Two extraction techniques, automatic southern apparatus, and conventional ultrasonic extraction, were compared in terms of yield, composition, and with special focus on antioxidant activity. In the DPPH test automated extraction showed higher antioxidant potential with an IC50 value of 7.5 mg/mL as compared to that of ultrasonic extraction which is 12.5 mg/L, whereas combining both was found to be relatively better. A similar trend in total phenolic and total flavonoid contents was observed. HPLC analysis of both extracts revealed the presence of gallic acid, p- p-hydroxybenzoic acid, caffeic acid, syringic acid rutin, and ferulic acid with significant differences in their profile.
- C. Urabee, Muthanna & Abdulsattar, Jwan & Nasif, Nayat & Al-Garawi, Zahraa. (2021). Extraction methods of Alhagi Maurorum (camel thorn) and its therapeutic applications. Journal of Physics: Conference Series. 1853. 012053. 10. 1088/ 1742- 6596/ 1853/ 1/ 012053.
- Chakou, Fatma Zohra & Boual, Zakaria & Ould, Mohamed & Hadj, El & Hakim, Belkhalfa & Bachari, K. & Alaoui-Talibi, Zainab & El Modafar, C. & Hadjkacem, Farah & Fendri, Imen & Abdelkafi, Slim & Traïkia, Mounir & Le Cerf, Didier & Dubessay, Pascal & Delattre, Cédric & Pierre, Guillaume & Michaud, Philippe. (2021). Pharmacological Investigations in Traditional Utilization of Alhagi maurorum Medik. in Saharan Algeria: In Vitro, Study of Anti-Inflammatory and Antihyperglycemic Activities of Water-Soluble Polysaccharides Extracted from the Seeds. Plants. 10. 10. 3390/ plants- 10122658. The anti-inflammatory and antihyperglycemic effects of polysaccharides extracted from Alhagi maurorum Medik. seeds and spontaneous shrubs collected in the Southern Algerian Sahara were investigated. Their water extraction followed by alcoholic precipitation was conducted to obtain two water-soluble polysaccharide extracts (WSPAM1 and WSPAM2). They were characterized using Fourier transform infrared, 1H/13C Nuclear Magnetic Resonance, Gas Chromatography-Mass Spectrometry, and Size Exclusion Chromatography coupled with Multi-Angle Light Scattering. The capacity of those fractions to inhibit α-amylase activity and thermally induced Bovine Serum Albumin denaturation were also investigated. WSPAM1 and WSPAM2 were galactomannans with a mannose/galactose ratio of 2.2 and 2.4, respectively. The SEC-MALLS analysis revealed that WSPAM1 had a molecular weight of 1.4 × 106 Da. The investigations highlighted antiinflammatory and antihyperglycemic effects in a dose-dependent manner of WSPAM1 and WSPAM2.
- Xu, Xiaoqin & Zhang, Juan & Chen, Liang & Sun, Yu & Qing, Degang & Xue-Lei, Xin & Yan, Chunyan. (2021). Alhagi pseudalhagi Extract Exerts Protective Effects Against Intestinal Inflammation in Ulcerative Colitis by Affecting TLR4-Dependent NF-κB Signaling Pathways. Frontiers in Pharmacology. 12. 10. 3389/ fphar. 2021. 764602. Alhagi pseudalhagi Desv. Extract (APE) is the major active fraction extracted from the aerial part of Alhagi pseudalhagi Desv. Because of its application in Uyghur medicine, it may be beneficial for the treatment of ulcerative colitis (UC). The present study aimed to investigate the possible beneficial effects of APE on UC mice and detect the possible mechanisms underlying these effects.
- Methods: An acute UC model was established in mice using dextran sulfate sodium. Sixty mice were randomly divided into six groups: normal, UC model, sulfasalazine (200 mg/kg), high-dose APE (APE- H, 2.82 g/ kg), middle-dose APE (APE- M, 1.41 g/ kg), and low-dose APE (APE- L, 0.70 g/ kg) groups. Drugs were administered by gavage for 10 days after the induction of colitis. Serum and colon tissue samples were collected from the mice during the experiment, and survival signs, body weight changes, disease activity index (DAI), colon length, and colon wet weight in mice were determined after the treatment. UC-induced damage, including inflammation and ulceration of colon mucosa, was observed by the naked eye as well as using hematoxylin and eosin staining (H&E) and scanning electron microscopy and scored according to Wallace and Keean’s criteria. We measured the levels of tumor necrosis factor α (TNF-α), interleukin (IL)- 1β, IL- 6, and IL- 10 in the serum and colon tissues using ELISA. Additionally, the relative protein levels of toll-like receptor 4 (TLR4), nuclear factor-kappa B p65 (NF-κB p65), phosphorylated NF-κB p65 at Ser536 (p-p65 Ser536), inhibitor kappa B-kinase ß (IK-Kβ), and phosphorylated IK-Kβ (Ser176/180) (p-IK-Kβ) in colonic mucosal epithelial tissues were detected using western blotting. The main functional components of APE were analyzed and confirmed by UPLC-MS/MS.
- Results: APE treatment repaired the UC-induced colon mucosa injury, reduced the weight loss, attenuated DAI, colon macroscopic damage index, and histological inflammation, and significantly downregulated the levels of inflammatory markers, including TNF-α, IL-1β, and IL-6, in the serum and colon tissues. Additionally, APE treatment reduced the levels of TLR4 and phosphorylation of p- NF- κB and p- IK- Kβ. The main components of APE are taxifolin, 3, 5- dihydroxy- 2- (4- hydroxyphenyl)- 7- [(2R, 3R, 4S, 5S, 6R)-3, 4, 5- trihydroxy- 6- (hydroxymethyl) oxen- 2- yl] polychrome- 4- one, hyperoside, rutin, kaempferol, isorhamnetin, 7, 8- dihydroxyflavone, and kaempferide.
- Shaker, Emad & Mahmoud, Hamdi & Mnaa, S. (2010). Anti-inflammatory and anti-ulcer activity of extract of Alhagi maurorum (Camel thorn). Food and chemical toxicology: an international journal published for the British Industrial Biological Research Association. 48. 2785- 90. 10. 1016/ j. ft. 2010. 07. 007.
- Bahamian, Nayere & Ahmadian, Shahin & Rafieian-kopaei, Mahmoud & Mobini, Gholam-Reza & Shafiezadeh, Mahshid & Soltani, Amin. (2021). A Comparative Study on Anticancer Effects of the Alhagi maurorum and Amygdalus haussknechtii Extracts Alone and in Combination with Docetaxel on 4T1 Breast Cancer Cells. Evidence-Based Complementary and Alternative Medicine. 2021. 1- 11. 10. 1155/ 2021/ 5517944. Medicinal plants have long been studied due to their anticancer effects and use is commonly increased as a complementary and alternative medicine (CAM therapies) among patients with cancer. In this study, Alhagi maurorum (A. m) and Amygdalus haussknechtii (A. h) extracts were evaluated for their effects on inhibiting the growth of 4T1 breast cancer cells. Based on MTT assay results, the IC50s of A.m and A.h extracts were 57 µg/ml and 85 µg/ml, respectively. Then the cell migration, gene expression, and degree of apoptosis after 48 hours in each treated group with A.m and A.h extracts alone or in combination with docetaxel (DTX) on 4T1 cells were evaluated. A.m had a synergistic behavior with DTX (CI 1. Cell migration assay showed that each extract alone or in combination with DTX prevented the migration of 4T1 cells. The Ao/EB staining and flow cytometry results confirmed that, in combination therapy, A.m + DTX and A.h + DTX induced apoptosis close to the level of DTX. Real-time PCR analysis showed that A.m + DTX (IC50 + IC25) downregulated the mRNA expression of HIF-1α and FZD7. A.m + DTX (IC50 + IC10) group decreased the expression of HIF-1α. Moreover, in the A.h + DTX (IC50 + IC25) group, β-Catenin and FZD7 were downregulated and upregulated, respectively. Generally, our findings suggest that the combination of A.m and DTX possesses synergistic antitumor effects on 4T1 cells, which may be a valuable choice for CAM therapies. A.h has an acceptable antitumor activity but not in combination with DTX.
- Sultan, A. & Moohammadnor, M. & Eshbakova, Komila. (2011). Chemical constituents of Alhagi pseudalhagi. Chemistry of Natural Compounds – CHEM NAT COMPD. 47. 140- 141. 10. 1007/ s10600- 011- 9860- 1.
- Rehman, Jalil & Akhtar, Naveed & Younus, Muhammad & Ahmad, Khalil & Ahmad, Mukhtiar & Sultana, Sabira & Asif, Muhammad. (2015). Phytochemical Screening and Hepatoprotective Effect of Alhagi maurorum Boiss (Leguminosae) Against Paracetamol-Induced Hepatotoxicity in Rabbits. Tropical Journal of Pharmaceutical Research. 14. 1029-1034. 10. 4314/ tjpr. v14i6. 13. Purpose: To evaluate the hepatoprotective activity of aqueous-ethanol (30: 70%) extract of Alhagi maurorum Boiss. (Leguminosae) whole plant against paracetamol-induced liver injury in experimental rabbits. Methods: Aqueous-ethanol extract of Alhagi maurorum at doses of 250 mg/kg and 500 mg/ kg body weight, p.o., was administered for 7 days in paracetamol (2 gm/ kg, s.c.) intoxicated rabbits and compared with silymarine (50 mg/ kg, p.o.)-treated rabbits. Biochemical parameters, alkaline phosphatase (ALP), serum glutamic oxalacetic transaminase (SGOT), serum glutamic pyruvic transaminase (SGPT), and total bilirubin (TB) levels were recorded to investigate the degree of improvement in the conditions of the rabbits. The liver was removed, washed with normal saline preserved in 10% formalin, and used in histopathological studies of hepatic architecture by microscopy. Phytochemical screening of the extract was also carried out. Results: The levels of biochemical parameters were increased in paracetamol-intoxicated rabbits when compared with the normal group. The extract, at doses of 250 and 500 mg/kg, exhibited a significant (p < 0.001) reduction in biochemical parameters (ALP, SGOT, SGPT, and TB). Hepatoprotective activity was also confirmed by histopathological findings. Furthermore, the phytochemical profile of the extract revealed the presence of tannins, alkaloids, saponins, and flavonoids. Conclusion: These results suggest that Alhagi maurorum extract possesses a significant hepatoprotective effect against paracetamol-induced hepatotoxicity and this may be due to the presence of flavonoids and tannins.
- Wagay, Nasir. (2016). Investigations on secondary metabolites of Alhagi pseudalhagi (M. Bieb.) Desv. ex B. Keller & Shap. Leaves using GC-MS. Investigations on secondary metabolites of Alhagi pseudalhagi (M. Bieb.) Desv. ex B. Keller & Shap. Leaves using GC- MS Wagay NA and Rothe SP Abstract Objective: To characterize the Phytoconstituents especially Secondary metabolites of Alhagi pseudalhagi (M. Bieb.) Desv. ex B. Keller & Shap. Leaves Using GC-MS. Methods: Qualitative phytochemical tests showed the presence of various compounds which were then verified by GC-MS analysis of Alhagi pseudalhagi (M. Bieb.) Desv. ex B. Keller & Shap. Leaves in Chloroform, 50% Ethanol and Dichloromethane solvents. Results: The GC-MS results of Chloroform extract showed the presence of fourteen compounds, ten compounds in 50% Ethanol extract, and seventeen compounds in Dichloromethane extract. Some fatty acids, hydrocarbons, and secondary metabolites were found in the extracts. The most important metabolites identified in Chloroform and Dichloromethane extract are Phenol, 2, 4- bis (1,1-dimethyl ethyl)- and Phytol; while in 50% Ethanol extract metabolites like Desulphosinigrin; β- D- Mannopyranoside, 1 -0- (10-undecyl)-; 3, 3′- Dimethyl- 1′- hydroxy- 5, 8- dimethoxy- 2, 2′- naphthalene-1, 4, 5′, 8′-tetrone and Stigmasterol. Conclusion: The compounds responsible for Anticancer, Antioxidant, Anti-inflammatory, and Antimicrobial were found to be present in the leaves.
- Muhammad, Gulzar & Asghar, Muhammad & Ahmad, Mushtaq & Kashmiri, Muhammad & Zia, Iram. (2011). Antioxidant and Antimicrobial Activities of Extracts from Aerial Parts of Alhagi pseudalhagi. Asian Journal of Chemistry. 23. 971- 976. In vitro, total antioxidant capacity and antimicrobial activity of aqueous and organic extracts from aerial parts of Alhagi pseudalhagi extracts were investigated. Initially, the antioxidant components were extracted in methanol and later subjected to partitioning in solvents of different polarity. Antioxidant and radical scavenging activity of these extracts were evaluated using antioxidant assays such as 2,2′- azinobis(3-ethylbenzothiazoline- 6- sulphonic acid) (ABTS) radical cation scavenging, 2, 2- diphenyl- 1- picrylhydrazil (DPPH) scavenging, total phenolic contents and total antioxidant activity determination using ferric thiocyanate method. Using ABTŠ+ decolorization assay A. pseudalhagi extracts showed a wide range of antioxidant activity. Trolox equivalent antioxidant capacity values ranged from 0.888- 5.525 mM of Trolox equivalents for different fractions of A. pseudalhagi. Using total phenolic contents and total flavonoid contents, the amount of total phenolics and flavonoids for different fractions of A. pseudalhagi ranged from 10. 657- 21.759 mg/ L of gallic acid equivalents (GAE) and 1.815- 10.911 mg/ L of quercetin equivalents, respectively. No significant correlation was found between total phenolic contents and trolox-equivalent antioxidant capacity values. Employing the potassium thiocyanate method, inhibition of lipid peroxidation comparable to trolox was exhibited by all the extracts. Antimicrobial activity of these extracts was also found against Bacillus subsites, Escherichia coli, Salmonella Typhimurium, Pseudomonas aeruginosa, and Aspergillus niger. Based on the results obtained here, A. pseudalhagi may be considered as a rich source of antioxidants and possesses potent antimicrobial activity.
- Mehina, Omer & Izzeldin, Omer & Abdalla, Rashid. (2014). In vivo study of Fagonia Cretica Linn toxicity in Sudan. International Journal of Pharmacology and Toxicology. 2. 104. 10. 14419/jpg. v2i2. 3594. Purpose: The study targeted to determine the toxicological effects of ethanolic extracts of Fagonia cretica linn plant in Khartoum, Omdurman, and Shendi towns in Sudan during (January – February) 2013. Objectives: To determine the LD50 of the plant and to study the effects of the plant on the body weight, vital organ weights, and anesthesia induction time effects. Methods: Different methods were adopted to achieve the objectives of this study, including Harborne methods for extraction. A total of (30), young adult Wistar rats, weighing (42.6 – 72.2) grams, fed standard rat food and water ad libitum, were maintained at standard laboratory conditions. All rats were grouped into (3) groups and survived the experiment by using the recommended progression doses of Fagonia cretica (175, 550, 1750, 5000, 5000, & 5000) mg/kg/body weight screenshot of AOT425 statistical program of main test. Toxicological studies in vivo (LD50 determination) were done in all (3) groups of animals that survived till the experiment was over after the administration of a selected high dose (5000) mg/ kg/ body weight. Ethical approval had been obtained from Omdurman Islamic University, Faculty of Pharmacy, and Department of Pharmacology under the number- (01/ 0/ 2013). Results: The LD50 is greater than 5000 mg/kg, indicating the high safety of the plant. The ethanolic extract of Fagonia cretica in doses of (100 & 300 mg/ kg/ body weight) has no effects on the rat’s relative vital organ weight (heart, liver, kidneys, lung, and spleen) during the study period of (14) days compared to the control group whilst the dose of (600) mg/ kg/ body weight change the liver somewhat from the relevant control, although, has no effects on the rats body weight during the study period of (14) days compared to the control group monitored at day (0, 7, 14). The anesthesia induction time on rats shows that the ethanolic extracts of the plant have a neurological effect on rats. Conclusion: The toxicological determination of LD50 was found to be greater than (5000) mg/ Kg, estimated by the special statistical software with three stopping criteria based on long-term outcomes. This indicates the wide safety margin of Fagonia ethanolic extract which encourages its use by humans for the treatment of many diseases.
Rasa Panchaka of Dhamasa
| Rasa (Taste) | Kashaya (Astringent), Tikata (Bitter), Madhura (Sweet), Katu (Pungent) |
| Guna (Virtue) | Laghu (Light), Snigdha (Oily) |
| Virya (Potency) | Sheet (Cold Potency) |
| Vipaka (Post-Digestion) | Madhura (Sweet) |
Dosha Karma of Dhamasa
Vata-Pitta Hara – Vata-Hara due to Madhura Vipaka and Pitta-hara due to Madhura Vipaka, Sheeta Virya and Madhura, Kashaya and Tikata Rasa.
Karma (Actions) of Dhamasa
Kustaghana, Jwaraghna, Visarpa Nashaka, Trishnahara, Bhrama Jit, Chardighana, etc.
Prayogarha Vyadhi (Therapeutic Indications) of Dhamasa
Jwara, Trishna, Daha, Rakta Pitta, Mada, Bhrama, Vata rakta, Kustha, etc.
Aamyik Paryog (Therapeutic Uses) of Dhamasa
Atisara (Diarrhoea): A paste of duralabha root the size of udumbara fruit should be taken along with the diet of milk processed with the same Duralabha Mula. (Sushruta Smahita Uttara Tantra. 40/ 74, 110)
Grahaniroga (IBS): Duralabhasava. (Charaka Samhita Chikitsa Sthana. 15. 152- 155)
Vertigo: To control vertigo, one should take a decoction of duralabh mixed with ghee. (Vrinda Madhava. 17. 7, Chakradutta. 17. 8, Vanga Sena. Murchha. 33, Bhava Parkasha Chikitsa. 19/ 40)
Chardi (Vomiting): Duralabha with honey should be taken to check for vomiting caused by kapha. (Charaka Samhita Chikitsa Sthana. 20/ 38, Ashtanaga Hridya Chikitsa Sthana. 6/ 21)
Mutraaghaat (Retention of urine): In this disorder, one should take the juice of duralabh or infusion of kumkum or every seed mixed with a little salt with water or milk cooked with pañcamula or simply grape juice. (Sushruta Samhita Uttara Tantra. 55/ 25, Ashtanga Hridya Chikitsa Sthana. 11/ 37, Vnaga Sena Udavartta. 17)
Rakta Pitta (Intrinsic hemorrhage): Duralabha is one of the drugs to be used with chanadana in various ways. (Charaka Samhita Chikitsa Sthana. 4. 75. 76)gu is the chief ingredient in Hingvadi Gutika (Sushruta Samhita Chikitsa Sthana. 5/ 2)
Benefits of Dhamasa on Different Systems of Bodies
External Uses:
- Dhamasa helps in alleviating swelling and pain. It has hemostatic action hence it is used in piles especially bleeding piles. Piles are cleaned with the decoction and the paste of the whole plant is applied over it. Patra Swarasa is used as a nasal drop for headache.
- Oil boiled with Dhamasa is used for massage in rheumatoid arthritis (Aamvata).
- Kwatha is used for gargling in stomatitis and for cleaning wounds. It prevents pus formation.
Nervous system: It has a tranquilizing effect on the brain hence it is used in symptoms like Bhrama, Murccha (syncope, vertigo), and brain weakness.
Digestive system: It is a Chardighana (antiemetic), antidiabetic, mild-laxative, and cholagogue. Therefore, it is used in emesis, dyspepsia, constipation, jaundice, and piles. Kapha and pitta work together in the lower part of the stomach.
Circulatory system: Dhamasa is a hemostatic and blood purifier, it is useful in hemorrhagic disorders and Vatarakta. Hot infusion (Phanta) of Dhamasa is given to prevent smallpox.
Respiratory system: It is used for common colds, coughs, and asthma as it acts as an expectorant and reduces the irritation of respiratory organs. Besides this, whole plants are used for smoking, and Kwatha is used for gargling in throat manifestations.
Mansavaha srotas: Dhamasa is applied over neck stiffness (Greeva Stambha).
Urinary system: It increases urination. A decoction is used in dysuria (Mutrakriccha).
Reproductive system: Being spermatogenic, it is given in semen debility.
Skin: It can be used for various skin disorders.
Temperature: Febrifuge and refrigerant by bitter and cold properties. The bitter taste is the best for fever.
Satmikaran: It increases physical strength and weight by unctuous and sweet properties.
Matra (Therapeutic Administration and Dosage) of Dhamasa
- Churna (Powder): 3-6 grams
- Kwatha (Decoction): 50-100 ml

Have A Health Issue?
Consult Online
- Dr. Sahil Gupta (B.A.M.S., M.H.A.)
Ayurvedic Allergy Specialist
CEO & Founder of IAFA®
Classical Reference of Dhamasa
Bhava Prakasha Nighantu Guduchyadi Varga- 211- 212
Synonyms
यासो यवासो दुःस्पर्शो धन्वयासः कुनाशकः |
दुरालभा दुरालम्भा समुद्रान्ता च रोदिनी |
गान्धारी कच्छुराऽनन्ता कषाया हरिविग्रहा ||
Bhava Prakasha Nighantu Guduchyadi varga 212- 214
Properties and action
यासः स्वादुः सरस्तिक्तस्तुवरः शीतलो लघुः |
कफमेदोमदभ्रान्तिपित्तासृक्कुष्ठकासजित् ||
यवासस्य गुणैस्तुल्या बुधैरुक्ता दुरालभा ||
Dhanwantri Nighantu Guduchyadi varga 20- 23
धन्वयासो दुरालम्भा ताम्रमूली च कच्छुरा |
दुरालभा च दुःस्पर्शा यासो धन्वयवासकः ||
दुरालम्भा स्वादुशीता तिक्ता दाहविनाशिनी |
विषमज्वरतृट्छर्दिमेहमोहविनाशिनी ||
Dhanvyasa Vishesha (Yasa)
यासो यवासकोऽनन्तो बालपत्रोऽधिकण्टकः |
दूरमूलः समुद्रान्तो दीर्घमूलो मरूद्भवः ||
यवासकः स्वादुतिक्तो ज्वरतृड्ररक्तपित्तनुत् ||
Kaiydeva Nighantu Aushadi Varga, 983- 986
दुरालभा दुरालम्भा धन्वयासो मरूद्रुवः ||
दूरमूलो दीर्घपत्रं समुद्रान्तो निकण्टकः |
यासो यवासो दुःस्पर्शो कच्छुरा ताम्रमूलिका ||
गान्धारिका बालपत्रानता धन्वयवासकः |
धन्वयासो हिमस्तिक्तः कषायो मधुरो लघुः ||
सरो निहन्ति पितास्रकफमेदोमदभ्रमान् |
विसर्पकुष्ठवातास्रतृष्णाकासवमिज्वरान् ||
Raja Nighantu Karviradi Varga. 53- 55
धन्वयासो दुरालम्भा ताम्रमूली च कच्छुरा |
दुरालभा च दुःस्पर्शा धन्वी धन्वयवासकः ||
प्रबोधनी सूक्ष्मदला विरूपा दुरभिग्रहा |
दुर्लभा दुष्प्रधर्षा च स्याच्चतुर्दशसञ्ज्ञका ||
दुरालम्भा कटुस्तिक्ता सोष्णा क्षाराम्लिका तथा |
मधुरा वातपित्तघ्नी ज्वरगुल्मप्रमेहजित् ||
Kshudra Durlbha (56- 58)
अन्या क्षुद्रदुरालम्भा मरुस्था मरुसम्भवा |
विशारदाऽजभज्ञा स्यादजादन्युष्ट्रभक्षिका ||
कषाया कफहृच्चैव ग्राहिणी करभप्रिया |
करभादनिका चेति विज्ञेया द्वादशाभिधा ||
दुरालम्भा द्वितीया च गौल्याम्लज्वरकुष्ठनुत् |
श्वासकासभ्रमघ्नी च पारदे शुद्धिकारिका ||
Priya Nighantu Shatpushpadi varga, 182
यास द्वयं सतिक्तम स्यात मधुरं शीतलाम लघु |
मद तृष्णा ज्वर छर्दि विसर्प भ्र्म कुष्ठ नुत ||
Vaidya amrita
यावसा धुमपानेन कासो नश्यति तत्क्षणात ||
Charaka Samhita Chikitsa Sthana. 14/ 100
दुःस्पर्शकेन बिल्वेन यवान्या नागरेण वा|
एकैकेनापि संयुक्ता पाठा हन्त्यर्शसां रुजम्||
Charaka Samhita Chikitsa Sthana. 14/ 196
दार्वी किराततिक्तं मुस्तं दुःस्पर्शकश्च रुधिरघ्नम्|
रक्तेऽतिवर्तमाने शूले च घृतं विधातव्यम्||
Charaka Samhita Chikitsa Sthana. 15/ 186-187
वत्सकातिविषे पाठां दुःस्पर्शां हिङ्गु चित्रकम्|
चूर्णीकृत्य पलाशाग्रक्षारे मूत्रस्रुते पचेत्||
आयसे भाजने सान्द्रात्तस्मात् कोलं सुखाम्बुना|
मद्यैर्वा ग्रहणीदोषशोथार्शःपाण्डुमान् पिबेत्||
इति चतुर्थक्षारः|
Charaka Samhita Sutra Sthana. 4/ 14 (30)
शटीपुष्करमूलबदरबीजकण्टकारिकाबृहतीवृक्षरुहाभयापिप्पलीदुरालभाकुलीरशृङ्ग्यइति दशेमानि हिक्कानिग्रहणानि भवन्ति |
Charaka Samhita Sutra Sthana. 4/ 15 (36)
Charaka Samhita Chikitsa Sthana. 3/ 197- 200
पाक्यं शीतकषायं वा मुस्तपर्पटकं पिबेत्||
सनागरं पर्पटकं पिबेद्वा सदुरालभम्|
किराततिक्तकं मुस्तं गुडूचीं विश्वभेषजम्||
पाठामुशीरं सोदीच्यं पिबेद्वा ज्वरशान्तये|
ज्वरघ्ना दीपनाश्चैते कषाया दोषपाचनाः||
तृष्णारुचिप्रशमना मुखवैरस्यनाशनाः|
Charaka Samhita Chikitsa Sthana. 4/ 75- 77
ह्रीबेरमूलानि पटोलपत्रं दुरालभा पर्पटको मृणालम्|
धनञ्जयोदुम्बरवेतसत्वङ्न्यग्रोधशालेययवासकत्वक्||
तुगालतावेतसतण्डुलीयं ससारिवं मोचरसः समङ्गा|
पृथक् पृथक् चन्दनयोजितानि तेनैव कल्पेन हितानि तत्र||
निशि स्थिता वा स्वरसीकृता वा कल्कीकृता वा मृदिताः शृता वा|
एते समस्ता गणशः पृथग्वा रक्तं सपित्तं शमयन्ति योगाः||
Charaka Samhita Chikitsa Sthana. 5/ 118- 121
जले दशगुणे साध्यं त्रायमाणाचतुष्पलम्|
पञ्चभागस्थितं पूतं कल्कैः संयोज्य कार्षिकैः||
रोहिणी कटुका मुस्ता त्रायमाणा दुरालभा|
कल्कैस्तामलकीवीराजीवन्तीचन्दनोत्पलैः||
रसस्यामलकानां च क्षीरस्य च घृतस्य च|
पलानि पृथगष्टाष्टौ दत्त्वा सम्यग्विपाचयेत्||
पित्तरक्तभवं गुल्मं वीसर्पं पैत्तिकं ज्वरम्|
हृद्रोगं कामलां कुष्ठं हन्यादेतद्घृतोत्तमम्||
इति त्रायमाणाद्यं घृतम्|
Charaka Samhita Chikitsa Sthana. 7/ 27(102- 103)
कुष्ठार्कतुत्थकट्फलमूलकबीजानि रोहिणी कटुका|
कुटजफलोत्पलमुस्तं बृहतीकरवीरकासीसम्||
एडगजनिम्बपाठा दुरालभा चित्रको विडङ्गश्च|
तिक्तालाबुकबीजं कम्पिल्लकसर्षपौ वचा दार्वी||
एतैस्तैलं सिद्धं कुष्ठघ्नं योग एष चालेपः|
उद्वर्तनं प्रघर्षणमवचूर्णनमेष एवेष्टः||
Charaka Samhita Chikitsa Sthana. 8/ 100
खर्जूरं पिप्पली द्राक्षा पथ्या शृङ्गी दुरालभा|
त्रिफला पिप्पली मुस्तं शृङ्गाटगुडशर्कराः||
Charaka Samhita Chikitsa Sthana. 14/ 153- 157
दुरालभायाः प्रस्थः स्याच्चित्रकस्य वृषस्य च|
पथ्यामलकयोश्चैव पाठाया नागरस्य च||
दन्त्याश्च द्विपलान् भागाञ्जलद्रोणे विपाचयेत्|
पादावशेषे पूते च सुशीते शर्कराशतम्||
प्रक्षिप्य स्थापयेत् कुम्भे मासार्धं घृतभाविते|
प्रलिप्ते पिप्पलीचव्यप्रियङ्गुक्षौद्रसर्पिषा||
तस्य मात्रां पिबेत् काले शार्करस्य यथाबलम्|
अर्शांसि ग्रहणीदोषमुदावर्तमरोचकम्||
शकृन्मूत्रानिलोद्गारविबन्धानग्निमार्दवम्|
हृद्रोगं पाण्डुरोगं च सर्वमेतेन साधयेत्||
इति द्वितीयफलारिष्टः |
Charaka Samhita Chikitsa Sthana. 16/ 47
कटुका रोहिणी मुस्तं हरिद्रे वत्सकात् पलम्|
पटोलं चन्दनं मूर्वा त्रायमाणा दुरालभा||४७||
कृष्णा पर्पटको निम्बो भूनिम्बो देवदारु च|
तैः कार्षिकैर्घृतप्रस्थः सिद्धः क्षीरचतुर्गुणः||४८||
रक्तपित्तं ज्वरं दाहं श्वयथुं स भगन्दरम्|
अर्शांस्यसृग्दरं चैव हन्ति विस्फोटकांस्तथा||४९||
इति कटुकाद्यं घृतम्||
Charaka Samhita Chikitsa Sthana. 20/ 38
सजाम्बवं वा बदराम्लचूर्णं मुस्तायुतां कर्कटकस्य शृङ्गीम्|
दुरालभां वा मधुसम्प्रयुक्तां लिह्यात् कफच्छर्दिविनिग्रहार्थम्||
Specific Formulation of Dhamasa
- Sudarshana Churna for Jwara and Yakrit Vriddhi
- Haritkyadi Kwatha for Vivandha and Mutra Kriccha
- Durlaha Kwatha for Bhrama
Contraindication and Side Effects of Dhamasa
The toxicological determination of LD50 was found to be greater than (5000) mg/ Kg, estimated by the special statistical software with three stopping criteria based on long-term outcomes of Fagonia cretica. This indicates the wide safety margin of Fagonia ethanolic extract which encourages its use by humans for the treatment of many diseases.
However, avoid the use of Dhamasa during pregnancy and lactation.
Suggestive Reading Regarding Dhamasa (Fagonia cretica)
- Miranda CL, Kumbi Y, Wu W, Lee HS, Reed RL, Stevens JF. Phytochemical characterization and bioactivity toward breast cancer cells of unhydrolyzed and acid-hydrolyzed extracts of Fagonia indica. Nat Prod Commun. 2022 Jul; 17 (7): 10. 1177/ 1934578. 221109426. doi: 10. 1177/ 1934578. 221109426. Epub 2022 Jul 5. PMID: 35875707; PMCID: PMC- 9302922.
- Lam M, Carmichael AR, Griffiths HR. An aqueous extract of Fagonia cretica induces DNA damage, cell cycle arrest, and apoptosis in breast cancer cells via FOXO3a and p53 expression. PLoS One. 2012; 7 (6): e40152. doi: 10.1371/ journal. phone. 0040152. Epub 2012 Jun 27. Erratum in: PLoS One. 2014 Jul; 9 (7): e102655. PMID: 22761954; PMCID: PMC 3384610.
- Ahmed W, Mansoor Q, Ahmad MS, Zainab T, Shah MA. TRAIL-mediated apoptosis ruling and anticancer triggered by fine-tuned nanospheres of Fagonia cretica methanolic extracts as novel cancer regime. Sci Rep. 2023 Jan 12; 13 (1): 671. doi: 10.1038/ s41598- 023- 27441-6. PMID: 36635434; PMCID: PMC9837038.
- Mahnashi MH, Alqahtani YS, Alyami BA, Alqarni AO, Ullah F, Wadood A, Sadiq A, Shareef A, Ayaz M. Cytotoxicity, anti-angiogenic, anti-tumor and molecular docking studies on phytochemicals isolated from Polygonum hydropiper L. BMC Complement Med Ther. 2021 Sep 24; 21 (1): 239. doi: 10. 1186/ s12906- 021-03411- 1. PMID: 34560864; PMCID: PMC- 8464109.
- Walbi, I. A., Alshabi, A. M., Alkahtani, S. A., Shaikh, I. A., A., B., Khateeb, M. M., Habeeb, M. S., Orabi, M. A., Shettar, A. K., & Hoskeri, J. H. (2023). A Preliminary Cytotoxicity Study of Fagonia arabica against Breast (MCF- 7), Oral (KB- 3- 1), and Lung Cancer (A- 549) Cell Lines: A Study Supported by Molecular Marker Analysis Using Dual Staining Dyes. Separations, 10 (2), 110. https:// doi. org/ 10. 3390/ separations- 10020110
- Rashid U, Khan MR, Sajid M. Hepatoprotective potential of Fagonia olivieri DC. against acetaminophen-induced toxicity in rats. BMC Complement Altern Med. 2016 Nov 9; 16 (1): 449. doi: 10. 1186/ s12906- 016- 1445- x. PMID: 27829418; PMCID: PMC- 5103455.
- Iqbal P, Ahmed D, Asghar MN. A comparative in vitro antioxidant potential profile of extracts from different parts of Fagonia cretica. Asian Pac J Trop Med. 2014 Sep; 7S1: S473- 80. doi: 10. 1016/ S1995- 7645 (14) 60277- 7. PMID: 25312170.
- Zulfiqar H, Zafar A, Rasheed MN, Ali Z, Mehmood K, Mazher A, Hasan M, Mahmood N. Synthesis of silver nanoparticles using Fagonia cretica and their antimicrobial activities. Nanoscale Adv. 2018 Dec 4; 1 (5): 1707- 1713. doi: 10. 1039/ c8na00343b. PMID: 36134229; PMCID: PMC- 9473189.
- Abrar A, Zafar A, Fatima M, Muntaqua D, Naz I, Fatima H, Ul Haq I. Mechanistic insight into the synergistic antimicrobial potential of Fagonia indica Burm. f. extracts with cefixime. Saudi Pharm J. 2024 Jan;32(1):101893. doi: 10.1016/ j. jsps. 2023. 101893. Epub 2023 Dec 5. PMID: 38204592; PMCID: PMC- 10777119.
- Nazir I, Ur Rahman N, Alvi Z, Hafizur Rahman M, Sendker J, Zhang T, Frankish N, Sheridan H. Antidiabetic Activities of an LC/MS Fingerprinted Aqueous Extract of Fagonia cretica L. in Preclinical Models. Planta Med. 2017 Oct; 83 (14- 15): 1141-1148. doi: 10.1055/ s- 0043- 107616. Epub 2017 Apr 7. Erratum in: Planta Med. 2017 Oct; 83 (14-15): E3. doi: 10. 1055/ s- 0043-109620. PMID: 28388787.
- Jafri L, Saleem S, Calderwood D, Gillespie A, Mirza B, Green BD. Naturally occurring TGR5 agonists modulate glucagon-like peptide-1 biosynthesis and secretion. Peptides. 2016 Apr; 78: 51-8. doi: 10. 1016/ j. peptides. 2016. 01. 015. Epub 2016 Jan 25. PMID: 26820940.
- Saleem S, Jafri L, ul Haq I, Chang LC, Calderwood D, Green BD, Mirza B. Plants Fagonia cretica L., and Hedera nepalensis K. Koch contain natural compounds with potent dipeptidyl peptidase- 4 (DPP- 4) inhibitory activity. J Ethnopharmacol. 2014 Oct 28; 156: 26- 32. doi: 10. 1016/ j. jep. 2014. 08. 017. Epub 2014 Aug 26. PMID: 25169215.
- Saad B, Kmail A, Haq SZH. Anti-Diabesity Middle Eastern Medicinal Plants and Their Action Mechanisms. Evid Based Complement Alternat Med. 2022 Jul 18; 2022: 2276094. doi: 10. 1155/ 2022/ 2276094. PMID: 35899227; PMCID: PMC- 9313926.
- Kamran S, Anwar R, Noor A, Ullah MI, Bagalagel AA, Aldurdunji MM, Ishtiaq S. Metabolic Profiling and Investigation of the Modulatory Effect of Fagonia cretica L. Aerial Parts on Hepatic CYP3A4 and UGT2B7 Enzymes in Streptozotocin-Induced Diabetic Model. Antioxidants (Basel). 2023 Jan 3; 12 (1): 119. doi: 10. 3390/ antiox- 12010119. PMID: 36670981; PMCID: PMC- 9854966.
- Khan HA, Ghufran M, Shams S, Jamal A, Khan A, Abdullah, Awan ZA, Khan MI. Green synthesis of silver nanoparticles from plant Fagonia cretica and evaluating its anti-diabetic activity through in-depth in-vitro and in-vivo analysis. Front Pharmacol. 2023 Oct 23; 14: 1194809. doi: 10. 3389/ fphar. 2023.1194809. PMID: 37936909; PMCID: PMC- 10625996.
- Khan HA, Ghufran M, Shams S, Jamal A, Ayaz M, Ullah M, Khan A, Khan MI, Awan ZA. In-depth in-vitro and in-vivo anti-diabetic evaluations of Fagonia cretica mediated biosynthesized selenium nanoparticles. Biomed Pharmacother. 2023 Aug; 164: 114872. doi: 10. 1016/ j. biopha. 2023. 114872. Epub 2023 May 26. PMID: 37245338.
- Nazar A, Adnan M, Shah SM, Bari A, Ullah R, Tariq A, Ahmad N. Ethnobotanical assessment of antidiabetic medicinal plants in District Karak, Pakistan. BMC Complement Med Ther. 2024 Apr 24; 24 (1): 173. doi: 10. 1186/ s12906- 024-04462- w. PMID: 38658923; PMCID: PMC- 11040872.
- Siddiqa A, Qureshi R, Raja NI, Khan IA, Ahmad MZ, Rafique S, Ali A, Ahmad A, Kaushik P. Liver-boosting potential: chicory compound-mediated silver nanoparticles for hepatoprotection-biochemical and histopathological insights. Front Pharmacol. 2024 Feb 21; 15: 1325359. doi: 10. 3389/ fphar. 2024. 1325359. PMID: 38449804; PMCID: PMC- 10914973.
- Almilaibary A, Abdallah EAA, El-Refaei MF. Fagonia indica attenuates chromium-induced nephrotoxicity via antioxidant and anti-inflammatory activities in mice. Heliyon. 2022 Aug 27; 8 (8): e10373. doi: 10. 1016/ j. heliyon. 2022. e10373. PMID: 36072257; PMCID: PMC 9441309.
- Qureshi H, Asif S, Ahmed H, Al-Kahtani HA, Hayat K. Chemical composition and medicinal significance of Fagonia cretica: a review. Nat Prod Res. 2016; 30 (6): 625- 39. doi: 10. 1080/ 14786419. 2015.1036268. Epub 2015 Apr 29. PMID: 25921950.
- Azam F, Sheikh N, Ali G, Tayyeb A. Fagonia indica Repairs Hepatic Damage through Expression Regulation of Toll-Like Receptors in a Liver Injury Model. J Immunol Res. 2018 Jul 2; 2018: 7967135. doi: 10. 1155/ 2018/ 7967135. PMID: 30057922; PMCID: PMC- 6051044.
- Satpute R, Bhattacharya R, S Kashyap R, J Purohit H, Y Deopujari J, M Taori G, F Daginawala H. Antioxidant Potential of Fagonia arabica against the Chemical Ischemia-Induced in PC12 Cells. Iran J Pharm Res. 2012 Winter; 11 (1): 303- 13. PMID: 24250453; PMCID: PMC- 3813090.
- Sajid, B. & Erum, Alia & Rizwana, K. & Uzma, Saeed, Alamgeer. (2011). Phytochemical screening and antimicrobial activity of Fagonia cretica plant extracts against selected microbes. J Pharm Res. 4. 962- 963.
- Khan HA, Ghufran M, Shams S, Jamal A, Khan A, Abdullah, Awan ZA, Khan MI. Green synthesis of silver nanoparticles from plant Fagonia cretica and evaluating its anti-diabetic activity through in-depth in-vitro and in-vivo analysis. Front Pharmacol. 2023 Oct 23; 14: 1194809. doi: 10. 3389/ fphar. 2023. 1194809. PMID: 37936909; PMCID: PMC- 10625996.
- Ahmed W, Mansoor Q, Ahmad MS, Zainab T, Shah MA. TRAIL-mediated apoptosis ruling and anticancer triggered by fine-tuned nanospheres of Fagonia cretica methanolic extracts as novel cancer regime. Sci Rep. 2023 Jan 12; 13 (1): 671. doi: 10.1038/ s41598- 023- 27441- 6. PMID: 36635434; PMCID: PMC- 9837038.
- Razi MT, Asad MH, Khan T, Chaudhary MZ, Ansari MT, Arshad MA, Saqib QN. Anti-hemorrhagic potentials of Fagonia cretica against Naja naja karachiensis (black Pakistan cobra) venom. Nat Prod Res. 2011 Dec; 25 (20): 1902- 7. doi: 10. 1080/ 14786419. 2010. 490785. Epub 2011 Nov 1. PMID: 21656416.
- Mehina, Omer & Izzeldin, Omer & Abdalla, Rashid. (2014). In vivo study of Fagonia Cretica Linn toxicity in Sudan. International Journal of Pharmacology and Toxicology. 2. 104. 10. 14419/jpg. v2i2. 3594.
Recent Research on Alhagi pseudalhagi / Alhagi camelorum
- Srivastava, Bhavana & Sharma, Himanshu & Dey, Yadu & Wanjari, Manish & Jadhav, Ankush. (2014). Alhagi pseudalhagi: a review of its phytochemistry, pharmacology, folklore claims, and Ayurvedic studies. International Journal of Herbal Medicine. 2. 47- 51.
- Xu X, Zhang J, Chen L, Sun Y, Qing D, Xin X, Yan C. Alhagi pseudalhagi Extract Exerts Protective Effects Against Intestinal Inflammation in Ulcerative Colitis by Affecting TLR4– Dependent NF- κB Signaling Pathways. Front Pharmacol. 2021 Nov 4; 12: 764602. doi: 10. 3389/ fphar. 2021. 764602. PMID: 34803708; PMCID: PMC- 8600043.
- Xu X, Zhang J, Chen L, Sun Y, Qing D, Xin X, Yan C. Alhagi pseudalhagi Extract Exerts Protective Effects Against Intestinal Inflammation in Ulcerative Colitis by Affecting TLR4-Dependent NF-κB Signaling Pathways. Front Pharmacol. 2021 Nov 4; 12: 764602. doi: 10. 3389/ fphar. 2021. 764602. PMID: 34803708; PMCID: PMC- 8600043.
- Bahamin N, Ahmadian S, Rafieian-Kopaei M, Mobini G, Shafiezadeh M, Soltani A. A Comparative Study on Anticancer Effects of the Alhagi maurorum and Amygdalus haussknechtii Extracts Alone and in Combination with Docetaxel on 4T1 Breast Cancer Cells. Evid Based Complement Alternat Med. 2021 Jun 14; 2021: 5517944. doi: 10. 1155/ 2021/ 5517944. PMID: 34221071; PMCID: PMC- 8219415.
- Ghavipanje, Navid, Einar Vargas-Bello-Pérez, Mojtaba Afshin, Seyyed Ahmad Hosseini, Alireza Aghashahi, and Amir Mansour Vatankhah. “The inclusion of Alhagi maurorum in growing camel diet: effect on Performance, Liver-Related Blood Metabolites, and Antioxidant Status.” Frontiers in Veterinary Science 9 (2022): 863121.
- Arman, Mohammad, Kazi Ashfaq Ahmed Chowdhury, Md Sazzadul Bari, Mohammad Forhad Khan, Maryam Md Ataul Huq, Md Areeful Haque, and Raffaele Capasso. “Hepatoprotective potential of selected medicinally important herbs: evidence from ethnomedicinal, toxicological and pharmacological evaluations.” Phytochemistry Reviews 21, no. 6 (2022): 1863- 1886.
- Singh, Shradhanjali, Alok Mukherjee, Shanti Bhushan Mishra, and Yogita Srivastava. “Assessment of the anti-arthritic potential of ethanolic extract and its fractions of aerial parts of Alhagi pseudalhagi (Bieb.) Desv. in animal models.” Oriental Pharmacy and Experimental Medicine 18, no. 3 (2018): 199- 208.
- Menze, E. T., Handoussa, H., Osman, A. K., Mostafa, N. M., & Swilam, N. (2021). UPLC-PDA-MS/MS Profiling and Healing Activity of Polyphenol-Rich Fraction of Alhagi maurorum against Oral Ulcer in Rats. Plants, 11 (3), 455. https:// doi. org/ 10. 3390/ plants. 11030455.
- Aierken, Aili, Zhihui Jiang, Kuerbanjiang Maimaitimin, Mikeremu Shayibuzhati, and Xiaoying Zhang. “Protective effect of Alhagi sparsifolia against acetaminophen-induced liver injury in mice.” Tropical Journal of Pharmaceutical Research 17, no. 4 (2018): 641- 646.
- Nishanbaev, S. Z., Kh M. Bobakulov, A. M. Nigmatullaev, I. D. Sham′ yanov, B. S. Okhundedaev, and N. D. Abdullaev. “Volatile compounds from the aerial parts of four Alhagi species growing in Uzbekistan.” Chemistry of Natural Compounds 52 (2016): 167- 170.
- Chakou FZ, Boual Z, Hadj MDOE, Belkhalfa H, Bachari K, El Alaoui- Talibi Z, El Modafar C, Hadjkacem F, Fendri I, Abdelkafi S, Traïkia M, Cerf DL, Dubessay P, Delattre C, Pierre G, Michaud P. Pharmacological Investigations in Traditional Utilization of Alhagi maurorum Medik. in Saharan Algeria: In Vitro, Study of Anti-Inflammatory and Antihyperglycemic Activities of Water-Soluble Polysaccharides Extracted from the Seeds. Plants (Basel). 2021 Dec 3; 10 (12): 2658. doi: 10. 3390/ plants10122658. PMID: 34961129; PMCID: PMC- 8704266.
- Saber TM, Abo- Elmaaty AMA, Said EN, Beheiry RR, Moselhy AAA, Abdelgawad FE, Arisha MH, Saber T, Arisha AH, Fahmy EM. Alhagi maurorum Ethanolic Extract Rescues Hepato- Neurotoxicity and Neurobehavioral Alterations Induced by Lead in Rats via Abrogating Oxidative Stress and the Caspase- 3- Dependent Apoptotic Pathway. Antioxidants (Basel). 2022 Oct 7; 11 (10): 1992. doi: 10. 3390/ antioxidant- 11101992. PMID: 36290715; PMCID: PMC- 9598489.
- Bahamian N, Rafieian-Kopaei M, Ahmadian S, Karimi I, Doustimotlagh AH, Mobini G, Bijad E, Shafiezadeh M. Combined treatment with Alhagi maurorum and docetaxel inhibits breast cancer progression via targeting HIF- 1α/ VEGF mediated tumor angiogenesis in vivo. Heliyon. 2023 May 15; 9 (5): e16292. doi: 10. 1016/ j. heliyon. 2023. e16292. PMID: 37234651; PMCID: PMC- 10205524.
- Khalifa HA, Shalaby SI, Abdelaziz AS. Alhagi maurorum aqueous extract protects against norfloxacin-induced hepato-nephrotoxicity in rats. Chin Herb Med. 2019 Dec 28; 12 (2): 156- 162. doi: 10. 1016/ j. Ahmed. 2019. 09. 007. PMID: 36119794; PMCID: PMC 9476674.
- Varshochi F, Asadollahi K. Alhagi; Traditional and modern medicine effective against kidney stones. J Nephropharmacology. 2015 Aug 26; 6 (1): 15- 16. PMID: 28197523; PMCID: PMC- 5295651.
- Xu X, Zhang J, Chen L, Sun Y, Qing D, Xin X, Yan C. Alhagi pseudalhagi Extract Exerts Protective Effects Against Intestinal Inflammation in Ulcerative Colitis by Affecting TLR4-Dependent NF-κB Signaling Pathways. Front Pharmacol. 2021 Nov 4; 12: 764602. doi: 10. 3389/ fphar. 2021. 764602. PMID: 34803708; PMCID: PMC- 8600043.
- Sagyndykova, M., Imanbayeva, A., Gassanova, G., & Ishmuratova, M. (2024). Current Status and Resources of Alhagi pseudalhagi (Fabaceae) in the Atyrau Region, Western Kazakhstan. Diversity, 16 (4), 219. https:// doi. org/ 10. 3390/ d16040219
References
- Agnivesha, Charaka, Dridhabala. In: Charaka Samhita, ed. Vaidya Jadavaji Trikamji Aacharya., editor. Varanasi: Chaukhamba Sanskrit Sansthan; 2009.
- Sushruta. In: Sushruta Samhita, Sutra Sthana, ed. Vaidya Jadavji Trikamji Acharya., editor. Varanasi: Choukhambha Orientalia; 2005.
- Vagbhata. In: Ashtanga Hrudaya, 9th ed. Anna Moreshwar Kunte, Krishnashastri Navarre, Harishastri, editors. Varanasi: Choukhambha Orientalia; 2005.
- Bhavamishra. In: BhavaPrakasha Nighantu, Guduchyadi Varga 11th ed. part 2. Brahma Shankara Mishra., editor. Varanasi: Choukhambha Bharati Academy; 2009.
- Bhavprakasha, commentary by Bulusu Sitaram, forwarded by K.C.Chunekar
- Sharma PV, Kaideva Nighantu. Aushadhi Varga. Chaukhamba Orientalia, Varanasi; 2006:
- Tripathi I., Raja Nighantu, Shahtavadi Varga Varga, Chaukhamba Krishnadas Academy; Varanasi; 2010
- Dhanwantri Nighantu, Guduchyadi Varga, Chaukhamba Krishnadas Academy; Varanasi.
- P.V. Sharma, Priya Nighantu, Shatpushpi Varga, Chaukhamba Krishnadas Academy; Varanasi.
- Shodhala Nighantu
- Dr. Gyanendra Pandey, Dravyaguna Vigyana, reprint 2012, Chawkhamba Krishnadas Academy
- K. Niteshwar Dravyaguna Vigyan, reprint 2017.
- Dr. J.L.N. Sastry and Dr. B.S. Sastry, Dravyaguna Vigyana, Chaukhambha Orientalia, Varanasi.
- Chakrapanidatta, Chakradatta with the vaidaya Prabha hindi commentary by indra deva tripathi, chaukambha sankrita sansthan, varanasi 2nd Edition, 1994.
Ayurveda is an Indian system of medicine that is popular since ancient times. Dr. Gupta’s IAFA® has been conducting research studies to find out different phytoconstituents of herbs and their action in the body. Such knowledge acquired by our experts is used in the preparation of medicines and providing the treatment facilities safely and effectively. IAFA® is the provider of safe and effective treatment for a wide range of diseases, mainly allergic diseases all based on Ayurveda.
Was this Page Helpful?
Read More Articles

Daruharidra (Berberis aristata)
Explore the uses, benefits, and medicinal properties of Daruharidra (Berberis aristata), also…

Haridra (Curcuma longa)
Discover the uses, benefits, and medicinal properties of Haridra (Curcuma longa), also…

Bhumi Amla (Phyllanthus Niruri)
Know the Uses, Benefits and Medicinal Properties of Bhumi Amla (Phyllanthus Niruri).…