On This Page
Aloe Vera: The Wonder Succulent Plant
Introduction
Ghrit Kumari botanically known as Aloe barbadensis is a succulent plant that grows in subtropical and arid climates. This plant grows to a height of 60- 100 cm and survives for 50 years under favorable conditions. This plant has been used traditionally since ancient times locally to reduce perspiration, orally for diabetes, and in various gastrointestinal disorders. The name Aloe vera for Kumari is derived from “Alloeh” an Arabic word that means shining bitter substance and Vera means true i.e true shining bitter substance. By the Greek scientist approximately 2000 years ago Kumari (Aloe vera) was considered the panacea. In Ayurvedic classical texts – Brihattrayi aloe vera is not mentioned. Shodhala first time mentioned the herb Kumari which means young girl. It is believed that Aloe vera brings femininity and youthful energy. Aloe vera has various potent chemical constituents like anthraquinones, saponins, amino acids, vitamins, minerals, etc due to which it exhibits antioxidant, anti-inflammatory, anti-fungal, anti-microbial, antiseptic, purgative properties, etc. In Ayurvedic classical texts, Kumari is mentioned as a blood purifier, uterine tonic, diuretic, laxative, antipyretic, etc.
Basonym of Kumari
कुमारयति क्रीड़ते स्वालेपन अपि जलेन शीतलत्वात् | कुमारीक्रीडायाम् वा ।
The plant which can survive with little quantity of water and it has a cooling effect.
Synonyms of Kumari
- According to Morphology:
स्थूलदला- स्थूलं दलम यस्या सा ।
Aloe vera (Kumari) has very big and thick leaves.
घृत कुमारी- घृत युक्ता कुमारी हति । दले दलिते सति घृतसमानरसस्य स्त्राविणीत्वात् ।
Leaves of Kumari have juice which resembles ghee.
विपुल स्रवा – विपुलं बहुस्राव॑ अस्त्यस्या: ।
On cutting the leaves it secretes more juices.
- According to action and properties:
कन्या- कनति कन्यते वा रसायनत्वातिगुणै: इति ।
Kumari possesses rejuvenating qualities and it is also very useful in disorders of teenage girls.
गृहकन्या- गृहे कन्या इव, माधुर्यादि गुणयुक्तत्वात् इति ।
The plant has got very good medicinal properties and is useful in disorders of teens, so liked by all people.
Regional Names of Kumari
- Indian aloe, Curacao Aloe, Barbados Aloe, Jaffarabad Aloe (English)
- Ghikanvar, Ghikuwar, Ghaikuwar, Gvarapatha, Dekvara (Hindi)
- Lolesara (Kannada)
- Kaattavala (Malayalam)
- Pivalaboel, Kuvargondal, Kourphad (Marathi)
- Patkvar (UP hills)
- Ghrit Kumari (Bengali)
- Kunwar Path (Gujrati)
- Chiruli (Tamil)
- Chimakat Banda (Telegu)
- Kumari (Malayalam)
- Sabbarat (Arabic)
- Darakhte Sibra (Persian)
Botanical Name
Aloe vera Tourn. ex. Linn.
Aloe’s name is derived from the Arabic word Alloeh- A
Family
Lilliaceae (Rasona Kula)
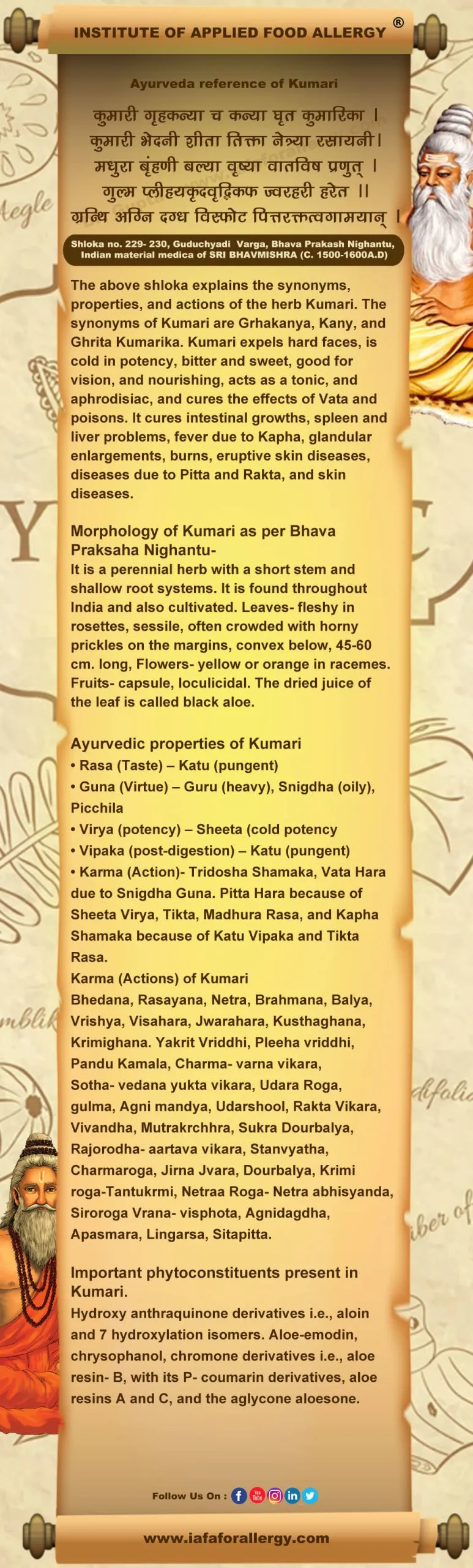
Ayurveda Reference for Kumari (Aloe vera Linn.)
Scientific Classification of Kumari
| Kingdom | Plantae |
| Class | Monocotyledons |
| Series | Coronariae |
| Family | Liliaceae |
| Genus | Aloe |
| Species | vera |
Classification of Kumari – As Per Charaka and Sushruta
- Charaka: Not mentioned in Mahakashaya
- Sushruta: Not mentioned in Gana
Dravya’s (Kumari) Description in Brihtrayi
There is no description of Kumari in Brihatryi.
Historical Background of Kumari
In Paniniya Grhya Sutras (1/ 21) we come across the mention of two kinds of Kumari (Kumari dvaya) but the botanical identity is not possible for the same. This plant is not mentioned by Brihattrayi. One plant Kanya described by Sushruta in the context of Rasayana is said to be a Soma-like powerful, magic herb that is different from Kumari. Dhanvantari Nighantu did not mention this plant while Sodhala for the first time introduced this plant into the Nighantus. It is interesting to note that it is the last drug mentioned in Kaiyadeva Nighantu. He considered Kumari as Vrishya as well as Rasayana. He specifically mentioned its flowers as Krimihara and Guru.
External Morphology of Aloe Vera
- Habit: Ghrita Kumari is a coarse-looking plant with a short stem, 1-2 feet high. The fleshy leaves (about 15 inches long, 4 inches broad, and 3/ 4 inches thick) are densely crowded. Large fleshy green leaves with sharp spines and white specks at the bases of the leaves. A perennial herb of about 30 cm. to 60 cm. high. Dwarf succulent plants up to 30-60 cm. in height.
- Stem: Short, thick, somewhat divided.
- Leaves: Leaves of Ghrita Kumari are sessile, thick, glaucous, aggregated, ensiform, 30-61 × 5-10 cm. with horny pickles/spiny toothed perpendicular or margin. Perianth is reddish yellow and green, cylindrical, 1.9- 2.5 cm.
- Fruit: Fruit is a loculicidal capsule.
- Leaf drug microscopy: Leaf epidermis full of stomata on both surfaces (as transverse section). Parenchyma rich in chlorophyll cells shows starch and bundles of needles of calcium oxalate. The central portion consists of mucilage containing parenchyma. A double row of vascular bundles located at the junction of the two preceding areas and with well-marked pericycle and endodermis.
- Dried juice (leaves): It varies in color from yellow-brown to chocolate brown. It breaks with a waxy fracture giving a sour odor. The taste is bitter. Drug shows (examined in lactophenol microscopically) crystals of aloin embedded in masses of resin.
Flowering and fruiting time
In Kumari, the plant flowering stage occurs during the winter and spring seasons.
Distribution of Kumari
The plant grows widely throughout India ascending to 1500 meters elevation in the Himalayan region. It is found in Africa, Arab, India, and China. The plant occurs in a semi-wild state in all parts from the dry westward valleys of the Himalayas up to Cape Comorin. Plants are generally propagated by suckers. Many of the forms of this species are naturalized.
Varieties of Kumari
Commercially there are four varieties of Kumari:
- Curacao aloes
- Cape aloes
- Socotrina aloes
- Zanzibar aloes
Useful Part of Kumari
Leaves
The juice obtained from the pulp of leaves when dried becomes a solid mass of irregular shape and different sizes, dark chocolate to black in a color surface is hard, and opaque with a slightly vitreous appearance. On breaking it becomes pieces exposing a glossy somewhat sticky surface. Thin pieces are translucent and brownish. It has a nauseating odor and bitter taste. Fresh juice is obtained by crushing the white pulp of green succulent leaves. It is a sticky liquid of golden yellow color having a nauseating odor and metallic taste.
Important Phytoconstituent of Kumari
Anthraquinone glycosides, aloin-barbaloin, iso barbaloin, B-barbaloin, aloe-emodin, resin, aloetic acid, homonataloin, aloesone, chrysophanic acid, chrysamminic acid, galacturonic acid, choline salicylate, mucopolysaccharides, glucosamine, and hexuronic acid.
Adulteration in Kumari
Black catechu, pieces of iron, and stones.
A Chemical Test of Kumari
Freshly prepared bromine solution is added to a small quantity of the filtrate prepared by 1 g of aloe powder boiled with 10 ml water and filtered with help of Kieselguhr. The test gives a pale-yellow precipitate of tetra-bromelain.
Recent Research on Kumari
- Aloe vera (A. V.) is a tropical plant with anti-inflammatory and immunostimulant effects, which could be of benefit in a diversity of wound healing conditions. This study aims to evaluate topically administered A. V. gel on oral cavity minor aphthous healing. It seems likely that A.V. 2% oral gel is not only effective in decreasing the recurrent aphthous stomatitis patient’s pain score and wound size but also decreases the aphthous wound healing period. Babaee N, Zabihi E, Mohseni S, Moghadamnia AA. Evaluation of the therapeutic effects of Aloe vera gel on minor recurrent aphthous stomatitis. Dent Res J (Isfahan). 2012 Jul; 9 (4): 381- 5.
- The present study aimed to investigate the anti-obesity effects of Aloe vera gel administration in male Sprague-Dawley (SD) rats with diet-induced obesity (DIO). SD rats at 7 weeks of age were fed either a standard diet (10 kcal% fat) (Std D) or high-fat (60 kcal% fat) diet (HFD) during the experimental period. The results suggest that intake of Aloe vera gel reduced body fat. accumulation, in part, by stimulation of energy expenditure. Aloe vera gel might be beneficial for the prevention and improvement of diet-induced obesity. Misawa E, Tanaka M, Nabeshima K, Nomaguchi K, Yamada M, Todia T, Iwatsuki K. Administration of dried Aloe vera gel powder reduced body fat mass in diet-induced obesity (DIO) rats. J. Nutr Sci Vitaminol (Tokyo). 2012; 58 (3): 195- 201.
- The present study was performed to explore the effect of an aqueous extract of Aloe vera on behavioral parameters of pain, Thus, the findings suggest that A. vera exerts its effect by a peripheral mechanism of action rather than central. Rathor N, Mehta AK, Sharma AK, Mediratta PK, Sharma KK. Acute effect of Aloe vera gel extract on experimental models of pain. Inflammation. 2012 Dec; 35 (6): 1900- 3. doi: 10. 1007/ 10753- 012- 9512- z.
- To investigate the anti-oxidative and anti-fibrotic effects of aloe vera in patients with liver fibrosis. Oral supplementation with AHM could help alleviate the fibrosis and inflammation of hepatic fibrosis patients. Hegazy SK, El- Bedewy M, Yagi A. Antifibrotic effect of aloe vera in viral infection-induced hepatic periportal fibrosis. World J. Gastroenterol. 2012 May 7;18 (17): 2026- 34. doi 10. 3748/ wig. v18. 117. 2026.
- Devaraj, Aruna & Karpagam, Thirunethiran. (2011). Evaluation of anti-inflammatory activity and analgesic effect of Aloe vera leaf extract in rats. Int. Res. J. Pharm.. 2. 103-110. Clinical evaluation of analgesic and anti-inflammatory drugs envisages the development of side effects that makes the efficacy of a drug arguable. Alternatively, the indigenous drug with fewer side effects is the major thrust area of research in the management of pain and inflammation. In the present study, an aqueous extract of the whole leaf of Aloe vera at various concentrations was investigated for its anti-inflammatory and analgesic activities in albino Wis
- tar rats. Carrageenan and formaldehyde-induced rat paw edema was used to evaluate the anti-inflammatory activity and tail flick, hot plate, and acetic acid tests were used to assess the analgesic activity of A. vera leaf aqueous extracts. Whole leaf aqueous extracts at various concentrations (100, 200, 400, and 600 mg/kg) significantly reduced the formation of edema induced by carrageenan and formaldehyde and granuloma formation in a dose-dependent manner. Further, the acetic acid-induced writhing model exhibited a significant analgesic effect characterized by a reduction in writhes. Whole leaf aqueous extract showed a dose-dependent increase in tolerance to thermal stimulus comparable to indomethacin. No mortality was observed during the acute toxicity test at a dosage of 600mg/kg. This whole-leaf aqueous extract of Aloe vera can be exploited as a non-toxic drug for the treatment and clinical management of inflammation and pain.
- The anti-inflammatory activity of Aloe vera was investigated through MMP inhibition studies. The effect of Aloe vera on MMP-9 inhibition was tested on peripheral blood mononuclear cells (PBMC). The inhibition of MMP-9 production in the cells was detected by gelatin zymography and was confirmed by RT- PCR. Vilayalakshmi D, Dhandapani R, Jayaveni S, Jithendra PS, Rose C, Mandal AB. In vitro anti-inflammatory activity of Aloe vera by downregulation of MMP-9 in peripheral blood mononuclear cells. J. Ethno-pharmacology. 2012 May 7; 141 (1): 542- 6. doi: 10. 1016/ j. jep. 2012. 02. 040. Pub 2012 Mar 15.
- Ferreira, Marcia & Teixeira, Marta & Silva, Elvira & Selores, Manuela. (2007). Allergic contact dermatitis to Aloe vera. Contact dermatitis. 57. 278-9. 10. 1111/ j. 1600- 0536. 2007. 01118. x. We present the case of a 72-year-old woman observed for dermatitis on the legs followed by the appearance of erythema on the eyelids. She had a history of peripheral venous insufficiency and had been using self-home-made Aloe vera juice over the legs for relief from pain. Patch tests showed positive reactions to the leaf of Aloe, the macerated Aloe jelly, and nickel sulfate. Although most manufacturers process Aloe products avoiding its irritant extracts, and probably as a consequence reports of allergic reactions are rare, one must remember that the growing popularity of the use of Aloe products may stimulate its use ‘as is’ by the patients.
- Sanchez, Marta & Gonzalez-Burgos, Elena & Iglesias, Irene & Gómez-Serranillos, Maria. (2020). Pharmacological Update Properties of Aloe Vera and its Major Active Constituents. Molecules (Basel, Switzerland). 25. 10.3390/molecules25061324. Aloe vera has been traditionally used to treat skin injuries (burns, cuts, insect bites, and eczemas) and digestive problems because of its anti-inflammatory, antimicrobial, and wound-healing properties. Research on this medicinal plant has been aimed at validating traditional uses and deepening the mechanism of action, identifying the compounds responsible for these activities. The most investigated active compounds are aloe-emodin, aloin, aloesin, emodin, and ace Mannan. Likewise, new actions have been investigated for Aloe vera and its active compounds. This review provides an overview of current pharmacological studies (in vitro, in vivo, and clinical trials), written in English during the last six years (2014-2019). In particular, new pharmacological data research has shown that most studies refer to anti-cancer action, skin and digestive protective activity, and antimicrobial properties. Most recent works are in vitro and in vivo. Clinical trials have been conducted just with Aloe vera, but not with isolated compounds; therefore, it would be interesting to study the clinical effect of relevant metabolites in different human conditions and pathologies. The promising results of these studies in basic research encourage a greater number of clinical trials to test the clinical application of Aloe vera and its main compounds, particularly on bone protection, cancer, and diabetes.
- The fertility rate of female rabbits was found to increase when 60 mg/kg or more of A. indica powder was given intragastrical (Sharma et al., 1972).
- Vazquez, Beatriz & Avila, Jose & Segura, David & Escalante, Bruno. (1997). Anti-inflammatory activity of extracts from Aloe Vera gel. Journal of Ethnopharmacology. 55. 69- 75. 10. 1016/ S0378- 8741 (96) 01476- 6. We studied the effects of aqueous, chloroform, and ethanol extracts of Aloe vera gel on carrageenan-induced edema in the rat paw, and neutrophil migration into the peritoneal cavity stimulated by carrageenan. We also studied the capacity of the aqueous extract to inhibit cyclooxygenase activity. The aqueous and chloroform extracts decreased the edema induced in the hind paw and the number of neutrophils migrating into the peritoneal cavity, whereas the ethanol extract only decreased the number of neutrophils. The anti-inflammatory agent’s indomethacin and dexamethasone also decreased carrageenan-induced edema and neutrophil migration. The aqueous extract inhibited prostaglandin E2 production from [14C] arachidonic acid. The chemical tests performed in the aqueous extract for glycosides, reductor sugars, and cardiotonic glycosides were positive. In the ethanol extract, the chemical tests performed for saponins, carbohydrates naphthoquinones, sterols, triterpenoids, and anthraquinones were also positive. In the chloroform extract, the chemical tests performed for sterols type delta 5, and anthraquinones were positive. These results demonstrated that the extracts of Aloe vera gel have anti-inflammatory activity and suggested its inhibitory action on the arachidonic acid pathway via cyclooxygenase.
- The expressed juice of A. vera, in the form of an ointment in Vaseline has been found to hasten the healing of wounds of thermal burns and radiation injury in albino rats. In addition, hydroxyproline and mucopolysaccharide contents were increased significantly in A. vera-treated animals (Singh et al., 1973).
- Hypoglycemic activity of polysaccharides yielded from the plant (A barbadensis) is reported (Hikino et al., 1983).
- Enzymes like carboxypeptidase are present in Aloe, which inactivate the bradykinin (which is responsible for inflammatory changes). Minerals like Mg inhibit histamine formation and hence aloe has antipruritic action. It contains vit. C, E, and Zn which are important for wound healing. Mannose-6-phosphatase is the major sugar in aloe that helps in wound healing (J. American Podiatry. Med. Assn. 1994 Feb.; 84: 77).
- The sugar present in aloe acts on the immune system. The anthraquinones exhibit an antimicrobial effect. The salicylic acid present in aloe has an anti-inflammatory and antibacterial effect. They also produce the Keratolytic effect. Out of 22 essential amino acids required for the human body, 20 are present in aloe. Aloe has an effect on the cytokine system causing immunomodulation (Marshal et al., 1993 & Green, 1996).
- Aloe increases the cross-linking of newly synthesized collagen tissue. The aqueous extracts of aloe have distinct anti-prostaglandin activity (analgesic activity) through inhibition of arachidonic acid, a cyclo-oxygenase 2 pathway. Aloe increases blood flow to the site of a wound. A. vera has 6 antiseptic agents (lupeol, salicylic acid, urea nitrogen, cinnamic acid, phenol & sulfur) – (Ind. J. Exp. Biol., 1998; 36: 896- 901).
- Aloe covers the open nerve endings to reduce pain sensation. Recent studies identified the role of aloe in patients with chronic leg ulcers (Nurse. Stand. 1998; 12: 49- 52).
- Gupta, Vivek & Kumar, Abhishek & Pereira, Maria & Siddiqi, Nikita & Sharma, Bechan. (2020). Anti-Inflammatory and Antioxidative Potential of Aloe vera on the Cartap and Malathion Mediated Toxicity in Wistar Rats. International Journal of Environmental Research and Public Health. 17. 10. 3390/ ijerph 17145177. Aloe vera has been the most useful medicinal herb in the world since ancient times due to its vast biological effects. The presence of high content of bioactive compounds makes Aloe vera a promising complementary and alternative agent in disease prevention. The effectiveness of A. vera-based medicines against pesticide toxicity has never been evaluated. It was therefore envisaged to develop an A. vera-based strategy to protect the non-target animals from the adverse effects of the pesticides. This article illustrates the ameliorating effect of aqueous extract (AE) of A. vera leaves against cartap and malathion toxicity. To evaluate the protective impact of A. vera against cartap (Ctp), malathion (Mtn), and a mixture of both pesticides, the animals were divided into eight groups, each containing six rats: Group 1- C (control), Group 2- AE + C, Group 3- Ctp, Group 4- Mtn, Group 5- Ctp + Mtn, Group 6- AE + Ctp, Group 7- AE + Mtn, Group 8- AE + Ctp + Mtn. Wistar rats exposed to Ctp, Mtn, and Ctp + Mtn, displayed a significant change in body weight. It was observed that the WBC level increased significantly in Mtn and Ctp + Mtn challenged groups. The contents of TNF-α and IL-6 in serum increased expressively in the Ctp, Mtn and Ctp + Mtn challenged groups. Rats treated with Ctp, Mtn, and Ctp + Mtn displayed significant alterations in the levels of antioxidative indices (MDA, GSH, GST, GPx, SOD, and CAT). Significant alterations were recorded in the activities of AST, ALT, ACP and ALP in Ctp, Mtn and Ctp + Mtn challenged groups. The histopathological results of the liver supported the biochemical data. The pre-treatment of rats with the aqueous extract of A. vera leaves significantly protected them from the toxicity of pesticides. These results suggested that A. vera extract may be used as a promising natural agent for the management of pesticide-induced toxicity.
- Guo, Xiaoqing & Mei, Nan. (2016). Aloe Vera – A Review of Toxicity and Adverse Clinical Effects. Journal of Environmental Science and Health, Part C. 34. 00- 00. 10. 1080/ 10590501. 2016. 1166826. The Aloe plant is employed as a dietary supplement in a variety of foods and as an ingredient in cosmetic products. The widespread human exposure and its potential toxic and carcinogenic activities raise safety concerns. Chemical analysis reveals that the Aloe plant contains various polysaccharides and phenolic chemicals, notably anthraquinones. Ingestion of Aloe preparations is associated with diarrhea, hypokalemia, pseudo melanosis coli, kidney failure, as well as phototoxicity and hypersensitive reactions. Recently, Aloe vera whole leaf extract showed clear evidence of carcinogenic activity in rats and was classified by the International Agency for Research on Cancer as a possible human carcinogen (Group 2B). This review presents updated information on the toxicological effects, including the cytotoxicity, genotoxicity, carcinogenicity, and adverse clinical effects, of Aloe vera whole leaf extract, gel, and latex.
- Aloe stimulates microcirculation in ulcers and wounds by increasing arteriolar diameter (J. Med. Asson. Thai. 2000; 83:417- 425).
- The application of aloe in second-degree burn wounds has produced excellent results (J. Med. Assn. Thai. 2000).
- Egesie, Ug & Chima, K.E. & Galam, Nanyak. (2011). Anti-inflammatory and analgesic effects of aqueous extract of aloe vera (Aloe barbadensis) in rats. African Journal of Biomedical Research. 14. 209-212. The anti-inflammatory and analgesic activities of the aqueous extract of Aloe barbadensis were investigated in rats. Formalin-induced hind paw edema was used to assess the anti-inflammatory activity of the extract while acetic acid-induced abdominal writhing was used for analgesic activity. The results of the anti-inflammatory study revealed that 25, 50, and 100 mg/kg of the extract reduced formalin-induced edema significantly (P<0.05) at the beginning of 3 hours when compared to the control group. In the analgesic study, 25, 50, and 100 mg/kg of the extract significantly (P<0.5) reduced the number of writhes induced by a 0.6% Acetic acid solution with approximately 66.49%, 57.59%, and 68.06% inhibition respectively. The present study showed that the aqueous extract of Aloe vera has anti-inflammatory and analgesic activities that could be mediated via modulators of pain and inflammation or through central activity. 2017, Ibadan Biomedical Communications Group. All rights reserved.
- Devaraj, Aruna & Karpagam, Thirunethiran. (2011). Evaluation of anti-inflammatory activity and analgesic effect of Aloe vera leaf extract in rats. Int. Res. J. Pharma 2. 103-110.
- Lee, Dajeong & Kim, Hyuk Soon & Shin, Eunju & Do, Seon-Gil & Lee, Chong-Kil & Kim, Young Mi & Lee, Min & Min, Keun & Koo, Jimo & Kim, Su & Nam, Seung & hyun woo, Kim & Park, Young Hwan & Choi, Wahn. (2018). Polysaccharide isolated from Aloe vera gel suppresses ovalbumin-induced food allergy through inhibition of Th2 immunity in mice. Biomedicine & pharmacotherapy = Biomedicine & pharmaco- therapy. 101. 201- 210. 10. 1016/j.biopha.2018. 02. 061. An allergic reaction occurs when the immune system overreacts to a harmless substance called an allergen that gains access to the body. Food allergy is a hypersensitive immune reaction to food proteins and the number of patients with a food allergy has recently increased. Aloe Vera is used for wellness and medicinal purposes. In particular, Aloe vera has been reported to enhance immunity. However, the effect of Aloe vera on food allergy is not yet known. In this study, we investigated the effects of processed Aloe vera gel (PAG) containing low molecular weight Aloe polysaccharide (AP) on ovalbumin (OVA)-induced food allergy in mice. Allergic symptoms, rectal temperature, and diarrhea were measured in OVA-induced food allergy mice. Other allergic parameters were also analyzed by RT-PCR, ELISA, flow cytometry, and other biochemical methods. As a result, PAG suppressed the decrease in body temperature, diarrhea, and allergic symptoms in OVA-induced food allergy mice. PAG also reduced serum concentrations of type 2 helper T cell (Th2) cytokines (Interleukin-(IL)-4, IL-5, and IL-13) as well as histamine, mast cell protease-1 (MCP-1), and immunoglobulin (Ig)E. PAG blocked the degranulation of mast cells and the infiltration of eosinophils in the intestine. Furthermore, PAG suppressed the population of Th2 cells in the spleen and mesenteric lymph nodes. PAG also increased the production of IL-10 and the population of type 1 regulatory T (Tr1) cells in mice with food allergies. Taken together, our findings suggest that PAG suppressed Th2 immune responses through, at least partially, stimulating the secretion of IL-10 in food allergy mice.
Rasa Panchaka of Kumari
| Rasa (Taste) | Katu (Pungent) |
| Guna (Virtue) | Snigdha (Oily), Guru (Heavy), Picchila |
| Virya (potency) | Sheeta (Cold Potency) |
| Vipaka (post-digestion) | Katu (Pungent) |
Dosha Karma of Kumari
Tridosha Shamaka, Vata Hara due to Snigdha Guna. Pitta Hara because of Sheeta Virya, Tikta, Madhura Rasa, and Kapha Shamaka because of Katu Vipaka and Tikta Rasa.
Karma (Actions) of Kumari
Bhedana, Rasayana, Netra, Brahmana, Balya, Vrishya, Visahara, Jwarahara, Kushta Ghana, Krimighana.
Prayogarha Vyadhi (Therapeutic Indication) of Kumari
Yakrit Vriddhi, Pleeha vriddhi, Pandu Kamala, Charma- varna vikara, Sotha- vedana yukta vikara, Udara Roga, gulma, Agni mandya, Udarshool, Rakta Vikara, Vivandha, Mutrakrchhra, Sukra Dourbalya, Rajorodha-aartava vikara, Stanvyatha, Charmaroga, Jirna Jvara, Dourbalya, Krimi roga-Tantukrmi, Netra Roga- Netra abhisyanda, Siroroga Vrana- visphota, Agnidagdha, Apasmara, Lingarsa, Sitapitta.
Aamyik Paryog (Therapeutic Uses) of Kumari
Pleeha Vriddhi (Spleen enlargement): The juice of kumari mixed with haridra powder alleviates splenomegaly and scrofula. (Sharangdhara Samhita. 2. 1. 15)
Apsmara (Epilepsy): Ghee cooked with kumari juice and decoction of madhuka and added with sugar is useful in epilepsy and palpitation of the heart. (Siddha Bhaishjya Mannimala. 4. 453)
Penile wart: Wrapping with the leaf of Kumari destroys the wart. (Raja Amrittanda. 24- 1, also BP. Ci. 52. 5)
Mutra Kriccha (Dysuria): If there is dysuria during fever, one should take the juice of kumari or decoction of light panchamula. (Vaidya Manorma. 7. 10)
Medra Shotha (Inflammation in the penis): Jiraka pounded with kumari juice is applied as a paste on the abscess. It pacifies burning sensation and inflammation. (Rasa Ratna Samucchya. 25. 18)
Vidridhi (Abscess):
- Kumari decocted with tila and sour gruel or alone ripens the abscess. (Vaidya Manorma. 16. 101)
- Unripe, ripening, or ripe abscesses should be covered with a steamed leaf devoid of pulp. (Vaidya Manorma. 16. 102)
Kamala (Jaundice): Kumari juice taken as snuff removes jaundice. (Bhava Parkasha Chikitsa. 8. 44)
Gulma:
- One suffering from gulma should swallow the pulp of kumari 5 gm mixed with cow-ghee and add a fine powder of trikatu, haritaki, and saindhava. (Bhava Parkasha Chikitsa. 32. 44)
- Kumari Asava. (YR. P. 268, Sharangdhara Samhita. 2. 10. 18- 27)
Mastitis: Kumari root mixed with haridra is applied as a paste on the breast to relieve pain. (Gada Nigreha. 6. 8. 23)
Shira Shoola (Headache): Kumari-tail. (BP. Ci. 62- 42- 48)
Anartava (Amenorrhoea): Kumarika vati, Rajahpravarttani vati. (BR. P. 1182-83) These contain extracts of kumari as kanyasara (aloe).
Benefits of Kumari
- The drug Kumari or Ghrita Kumari is bitter, Cathartic, anthelmintic, aphrodisiac, cooling, emmenagogue, hepatic stimulant, purgative, and vermifuge.
- It is used in indigenous medicine for hemophilic, skin, and uterine disorders. Locally it is applied on burns.
- It is also used in cosmetics for application over the face and skin. The drug is topically applied to ulcers, wound eruptions, or eruptive boils. It is used in anemia, jaundice, liver, and splenic disorders, menstrual troubles, worms, chronic fever, dysuria, edema, abdominal disorders, inflammatory and painful complaints (organs), colic, poisons, and general debility.
- It is a blood purifier, tonic, and wholesome to the eyes.
- The drug is restorative (Rasayana) and it is useful in urticaria, headache, loss of appetite, leucorrhea, and constipation; it allays Vata and kapha besides its cholagogue action.
- The drug is frequently recommended for gynecological complaints. It is used as a single drug, recipe, and compound formulation.
- Besides being an ingredient of several pharmaceutical preparations (compounds), the plant drug is employed in some processes of pharmacy (rasa shastra and bhaishajya kalpana) in Indian medicine. It is utilized in shodhana and Marana methods (process) of certain processes and preparations.
- In addition to pharmaceutical formulations of the classical group (Sastriya) as well as new herbo- mineral products indicated in the treatment of various diseases.
- The plant drug Kumari is the major ingredient of Kumaryasava, Rajahpravartani vati, Kumarika vati, Kumari tail, Kumaripaka, etc. incorporated in Indian medicine.
- Some other drug preparations are made in Unani medicine. Kanyasara or Aloes (extract) or Musabbar is used in medicine for treating different ailments and it is also an ingredient of medicinal preparations used externally and internally in therapeutics.
- Kumari has been an important and potent drug in ancient medicine and therapeutics, finding its uses in several diseases as mentioned in different classical texts dealing with clinical management.
- The juice of Kumari leaves (pulp) is taken as a snuff which is useful to relieve jaundice or Kamala.
- Kumari nasya is referred to by Bhavamisra (Bhavaprakasa, chikita. 8- 44). Kumar is used in jaundice and anemia (Kamala and pandu) in other forms also since its pharmacological actions on liver and spleen function.
- Kumar leaves are used in enlargements and other disorders of the liver and spleen in the body. Kumari is a potent cholagogue drug (pitta-nirharana- pitta- rechana).
- The juice of Kumari mixed with Haridra (turmeric) powder is given in spleen enlargement or pliha vriddhi (Sarangadhara Samhita, 2- 1- 15).
- In the therapeutic management of amenorrhoea (rajorodha), the extract of Kumari leaves juice or Kanyasara (aloe) is the chief ingredient of two compounds viz. Kumarikavati and Rajahpravartani vati are frequently prescribed for menstrual problems as emmenagogue drugs (Bhaisajya Ratnavali, p-1182-1183).
- Kumarya Asava is another prominent classical formulation that is generally recommended for female diseases and also other ailments.
- Kumari is mixed with tila and sour gruel or alone applied to ripen the abscess. Kumari leaves or juice is recommended to apply over abscesses and wounds in Ama and pacyamana stages for attaining pakva condition of vidradhi and Vrana (Vaidya Manorama, 16- 101- 102).
- Leaves pulp of Kumari are prescribed to externally apply over or by covering up with the steamed leaves devoid of pulp, in all stages of abscess as indicated in medical texts (Vidradhi chikitsa contexts).
Benefits of Kumari on Different Systems of Bodies
External use: As Poultice because it exhibits anti-inflammatory action, can be applied on inflamed parts. Kala bol powder can be applied to small wounds. A warm paste of kumari juice with turmeric churna can be applied over the swollen, painful, and enlarged spleen. Juice can be used in the eyes for conjunctivitis. In headaches and eye problems, the pulp can be applied locally. The juice is refrigerant.
Digestive system:
- In small doses, kumari has deepan, pachan, bhedan, and uttejak properties. In large doses, it is virechaka and krimighna. It increases the secretions of the small intestine and promotes the peristalsis of the large intestine. Since its action is slow, the laxative effect is observed after 10-12 hours. If taken in excess quantity, rational action is not observed but ill effects in the form of gripping, constipation and sometimes bleeding are observed. In moderate quantities, stools are observed to be soft and solid and dark colored. There is increased congestion in the anal region due to the consumption of kumari.
- Very often it may result in information of piles.
- Juice of kumari is useful in loss of appetite, ascites, tumors, liver and spleen enlargement, and abdominal colic.
- It is laxative, anti- flatulent.
Cardiovascular system: It is yakrit gami, rakta vaha srotogami, and is useful in the purification of blood and affections of the liver. It is used in splenomegaly in combination with haridra.
Urogenital system: It is a known diuretic. Snigdha and pichchil promote the secretion of semen and act as an aphrodisiac. Being ushna, it increases the flow of blood to the uterus and promotes contraction as a result of which leads to uterine bleeding. Hence kala bol is used locally for the treatment of amenorrhoea.
Skin: Useful in common conditions of the skin, it promotes hair growth.
Temperature: It is useful in chronic fevers.
Satmikaran: Kumari juice or kala bol can be used as a restorative in generalized weakness. It is a tonic. The juice is anabolic and increases strength.
Matra (Therapeutic Administration and Dosage) of Kumari
- Juice of leaves (Patra Swarasa)- 10- 20 ml
- Kala Bol- 1- 4 Ratti

Have A Health Issue?
Consult Online
- Dr. Sahil Gupta (B.A.M.S., M.H.A.)
Ayurvedic Allergy Specialist
CEO & Founder of IAFA®
Classical Reference of Kumari
Bhava Prakasha Nighantu Guduchyadi Varga- 229
Synonyms
कुमारी गृहकन्या च कन्या घृत कुमारिका ।
Bhava Prakasha Nighantu Guduchyadi Varga- 229- 230
Properties and Actions
कुमारी भेदनी शीता तिक्ता नेत्र्या रसायनी।
मधुरा बृंहणी बल्या वृष्या वातविष प्रणुत् ।
गुल्म प्लीहयकृदवृद्धिकफ ज्वरहरी हरेत ।।
ग्रन्थि अग्नि दग्ध विस्फोट पित्तरक्तत्वगामयान् |
Kaiydeva Nighantu Aushadi Varga, 1639- 1640
कुमारी शीतला तिक्ता मधुरा भेदनी जयेत् ।
गुल्मप्लीह: यकृदवृद्धि कफज्वरहरी हरेत ।
ग्रंथि अग्नि दग्ध विस्फोट पित्तरक्तत्वगामयान ।।
चक्षुष्य विषवातघ्ती बल्या वृष्या रसायनी ।
Raja Nighantu Parpatadi varga, 49
गृहकन्या हिमा तिक्ता मदगन्धि कफापहा ।
पित्त कास विष श्वास कुष्ठ्घ्नी च रसायनी ||
Priya Nighantu Shatpushpadi Varga, 154- 155
कुमारी मधुरा तिकता सरा शीता रसायनी |
गुल्म प्लीहा यकृद व्रृद्धि रजोरोधान विनाश्येत |
अन्य च रोगा नश्यन्ति कुमार्यासव सेवनात |
Kaiydeva Nighantu Aushadi Varga, 1640
कुमारी पुष्पम्
वात पितकृमिहरं कुमारी कुसुमं गुरु |
Bhava Prakasha Nighantu Guduchyadi Varga- 221- 230
कुमारी भेदिनी शीता तिका मेध्या रसायनी ||
मधुरा बृहणी बल्या वृष्यावात विषप्रणुत् |
गुल्मप्लीहयकृदवृद्धि कफ ज्वरहरी हरेत् ||
ग्रंथि अग्नि दग्ध विस्फोट पित्तरक्तत्वगामयान् ||
Raja Nighantu
गृहकन्या हिमा तिका मद्गन्धि: कफापहा |
पित्त कास विष श्वास कुष्ठ्घ्नी च रसायनी ||
Atharva Veda
वीरा स्त्राव: सहसार: कुमारी सम्भव: |
सहासारो अग्नि जनन: पित्तनिहरणोमत: ||
बलकृद्रेचन: पुष्पजननों गर्भपातन: |
विट्सज्ञे कृमिरोगे च संन्यासे अपस्मृतौ तथा |
लुप्ते रजसि नारीणां शीतपित्ते शिरोरुजि |
ज्वरे श्लेष्मोद्भवे प्लीहि मन्द अग्नौ च प्रयुज्यते ||
अर्शसस्त॑ न सेवेत नान्तर्वत्नी न पुष्पिणी |
न च असृग्दरिणी नापि यकृद्वृ क्कादि रोगवान् ||
Bhava Prakasha Pandu Kamala Halimaka Adhikaram, 32- 44
कामलारोगे घृतकुमारी नस्यम्
अपहरति कामला अर्ति नस्येन कुमारिकाजलं सद्य: |
Bhava Prakasha Gulma Adhikara, 32- 44
गुल्मे कुमारिका मांसम्
गुल्मी कुमारिकामांसं कर्षाद्ध गोघृतान्वितम् |
Bhava Prakasha Madhya Khanda, 52- 5, Rajaa Mastaanda, 24- 1
लिंग अर्श घृतकुमारी लेपम
हरति घृतकुमारी पलमावेष्नेन ग्रथन विद्धि विशेषां चर्म कीला स्तृतीये |
अहनि गुरुतरानप्यद्वब्धप्रतिष्ठान् विधिरिव विपरीत: पौरुषस्य प्रकारान् ||
Bhava Prakasha Shiro Roga Adhikara, 62- 42/ 48
शरोरोगादयः चिकित्सायाम्
कुमारी तैलम्
रजोरोधो
कुमारिकावटी
रज:प्रवर्त्तिनीवटी
Vaidya Manorma, 7- 10
मूत्र कृच्छ
ज्वरेषु मूत्रकृच्छ॑ चेत् कुमारी स्वरसं पिबेत् |
कन्नीय: पंचमूलम वा गुह्यमेतच्चिकित्सितम् ||
Gada Nigreha, 6- 8- 23
स्तन व्यथायाम
स्त्रीणां हरिद्रा सहितं कुमारी मूलं विशालाप्रभवं कदाचित् ||
Sharangdhara Samhita
प्लीहा वृद्धौ
निशा चूर्ण युत: कन्यारस: प्लीहापचीहर: |
Siddha Bhaishjya Mannimala, 4- 453
अपस्मार
मधुक क्वाथ सहिते कुमारी स्वरसे श्रृतम |
घृतम स्मृतमपस्मारे हदुत्फाले सशर्करम् ||
Rasa Ratna Samuuchya, 25- 18
वर्णे
कुमाई समपिष्टम जीरकम लेपयेद भिषक्।
तेन दाहश्च पाकश्च शमाप्राप्नोति निश्चितं ||
Vaidya Manorma, 16- 101- 102
तिल आरनाल कवथिता कुमारी पाचयेद् व्रणान् |
केवला अथ कुमारी वा पक्वापक्व विशंकितान |
आमे वा पच्यमाने वा पक्वे वा कन्यकां वर्णे |
स्वीना विनिर्गन्त्रा च निक्षेपेत सामप्रशाम्यति |
Vishista Yoga (Name of Important Formulation)
Kumari Taila for Manda Agni, Snayu Vikara
Kumari taila for Ardita and Shiro Roga
Raja Pravartini Vati for Rajo Rodha, Kasta Aartava
Kumari Asava for Kasa and Swasa
Kumari Paka
Contraindication and Side Effects of Kumari
Some common side effects of Kumari are hypoglycemia, stomach pain, Kidney problems, diarrhea, muscle weakness, weight loss, etc.
The study revealed that taking lates of aloe vera more than 1 gram per day for several days can result in kidney failure. So it is recommended to consult your doctor before its use.
Oral use of latex of Kumari is contraindicated for children below 12 age.
Adverse Clinical Effect of Kumari Gel (Aloe Vera Gel) on Humans
Reference: Guo X, Mei N. Aloe vera: A review of toxicity and adverse clinical effects. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 2016 Apr 2; 34 (2): 77- 96. doi 10. 1080/ 10590501. 2016. 1166826. PMID: 26986231; PMCID: PMC 6349368.
Aloe gels were first used clinically in the 1930s for the treatment of radiation burns. Afterward, several clinical trials of Aloe vera gel have been carried out in the treatment of burn wounds, oral lichen planus, hyperlipidemic type 2 diabetic patients, and recurrent aphthous stomatitis. Only some minor adverse effects were reported in these studies, such as discomfort, pain, and the development of hypersensitive reactions. However, generalized eczematous and papular dermatitis was found in a male patient in response to the oral and topical use of the Aloe vera gel. Pruriginous erythema was observed on the legs and eyelids of a 72-year-old woman after applying self-made Aloe vera leaf juice over the legs. A very slow recovery from dermatitis induced by Aloe vera preparations was reported in four cases after dermabrasion and chemical peel. No severe adverse effects or carcinogenicity have been reported from using Aloe vera gel.
Suggestive Reading Regarding Aloe vera
- Christaki, Efterpi & Florou-Paneri, Panagiota. (2010). Aloe vera: A plant for many uses. Journal of Food, Agriculture, and Environment. 8.
- Itrat, Malik & Zarnigar, (2013). ALOE VERA: A REVIEW OF ITS CLINICAL EFFECTIVENESS. INTERNATIONAL RESEARCH JOURNAL OF PHARMACY. 4. 75- 79. 10. 7897/ 2230- 8407. 04812.
- Pegu, Arup & Sharma, Mrs. (2019). Review on Aloe Vera. International Journal of Trend in Scientific Research and Development. Volume-3. 35- 40. 10. 31142/its 23541.
- Gupta, Vivek & Kumar, Abhishek & Pereira, Maria & Siddiqi, Nikita & Sharma, Bechan. (2020). Anti-Inflammatory and Antioxidative Potential of Aloe vera on the Cartap and Malathion Mediated Toxicity in Wistar Rats. International Journal of Environmental Research and Public Health. 17. 10. 3390/ ijerph 17145177.
- Vázquez, Beatriz & Avila, Jose & Segura, David & Escalante, Bruno. (1997). Antiinflammatory activity of extracts from Aloe Vera gel. Journal of Ethnopharmacology. 55. 69- 75. 10. 1016/ S0378- 8741 (96) 01476- 6.
- Alvarez-Perea, Alberto & Prieto-García, Alicia & Hernandez, Alejandro & de Barrio Fernandez, Manuel & Baeza, Maria. (2010). Urticaria due to aloe vera: A new sensitizer? Annals of Allergy, Asthma & Immunology: official publication of the American College of Allergy, Asthma, & Immunology. 105. 404- 5. 10. 1016 /j. Anai. 2010. 09. 016.
- Hashemi SA, Madani SA, Abediankenari S. The Review on Properties of Aloe Vera in Healing of Cutaneous Wounds. Biomed Res Int. 2015; 2015: 714216. doi 10. 1155/ 2015/ 714216. Epub 2015 May 19. PMID: 26090436; PMCID: PMC 4452276.
- Ahlawat KS, Khatkar BS. Processing, food applications and safety of aloe vera products: a review. J Food Sci Technol. 2011 Oct; 48 (5): 525- 33. doi 10. 1007/ s13197- 011- 0229- z. Epub 2011 Jan 18. PMID: 23572784; PMCID: PMC 3551117.
- Hamman JH. Composition and applications of Aloe vera leaf gel. Molecules. 2008 Aug 8; 13 (8): 1599- 616. doi 10. 3390/ molecules 13081599. PMID: 18794775; PMCID: PMC 6245421.
- Ferreira, Márcia & Teixeira, Marta & Silva, Elvira & Selores, Manuela. (2007). Allergic contact dermatitis to Aloe vera. Contact dermatitis. 57. 278- 9. 10. 1111/ j. 1600- 0536. 2007. 01118. x.
- Maharjan R, Nagar PS, Nampoothiri L. Effect of Aloe barbadensis Mill. the formulation on Letrozole induced polycystic ovarian syndrome rat model. J Ayurveda Integr Med. 2010 Oct; 1 (4): 273- 9. doi: 10. 4103/ 0975- 9476. 74090. PMID: 21731374; PMCID: PMC 3117319.
- Hes M, Dziedzic K, Gorecka D, Jędrusek-Golinska A, Gujska E. Aloe vera (L.) Webb.: Natural Sources of Antioxidants – A Review. Plant Foods Hum Nutr. 2019 Sep; 74 (3): 255- 265. doi 10.1007/ s11130- 019- 00747- 5. PMID: 31209704; PMCID: PMC 6684795.
- Guo X, Mei N. Aloe vera: A review of toxicity and adverse clinical effects. J Environ Sci Health C Environ Carcinogen Ecotoxicology Rev. 2016 Apr 2; 34 (2): 77- 96. doi 10. 1080/ 10590501. 2016. 1166826. PMID: 26986231; PMCID: PMC 6349368.
- Hekmatpou D, Mehrabi F, Rahzani K, Aminiyan A. The Effect of Aloe Vera Clinical Trials on Prevention and Healing of Skin Wound: A Systematic Review. Iran J Med Sci. 2019 Jan; 44 (1): 1- 9. PMID: 30666070; PMCID: PMC 6330525.
- Sánchez M, González-Burgos E, Iglesias I, Gómez-Serranillos MP. Pharmacological Update Properties of Aloe Vera and its Major Active Constituents. Molecules. 2020 Mar 13; 25 (6): 1324. doi: 10. 3390/ molecules 25061324. PMID: 32183224; PMCID: PMC 7144722.
- Lee, Dajeong & Kim, Hyuk Soon & Shin, Eunju & Do, Seon-Gil & Lee, Chong-Kil & Kim, Young Mi & Lee, Min & Min, Keun & Koo, Jimo & Kim, Su & Nam, Seung & hyun woo, Kim & Park, Young Hwan & Choi, Wahn. (2018). Polysaccharide isolated from Aloe vera gel suppresses ovalbumin-induced food allergy through inhibition of the immunity in mice. Biomedicine & pharmacotherapy Biomedicine & pharmacotherapy. 101. 201- 210. 10. 1016/ j. biota. 2018. 02. 061.
- Adams K, Eliot T, Gerald A. Extent of Use of Aloe vera Locally Extracted Products for Management of Ailments in Communities of Kitagata Sub-County in Sheema District, Western Uganda. Int J Sci Basic Appl Res. 2014; 15 (1): 1-15. PMID: 26855960; PMCID: PMC 4737949.
- Egesie, Ug & Chima, K.E. & Galam, Nanyak. (2011). Anti-inflammatory and analgesic effects of aqueous extract of aloe vera (Aloe barbadensis) in rats. African Journal of Biomedical Research. 14. 209- 212.
- Radha MH, Laxmi Priya NP. Evaluation of biological properties and clinical effectiveness of Aloe vera: A systematic review. J Tradit Complement Med. 2014 Dec 23; 5 (1): 21- 6. doi: 10.1016/ j. jtcme. 2014.10. 006. PMID: 26151005; PMCID: PMC 4488101.
- Kamil, Mohammad. (2020). Anti-Inflammatory and Anti-Obesity Activities of Aloe Vera. Open Access Journal of Complementary & Alternative Medicine. 2. 10. 32474/ OAJCAM. 2020. 02. 000131.
- Bohra A, Maheswari TNU, Harsh A, Garg A. Black Turmeric and Aloe Vera in the Management of Oral Submucous Fibrosis: A Prospective Clinical Study. Asian Pac J Cancer Prev. 2021 Dec 1; 22 (12): 3941- 3947. doi 10. 31557/ APJCP. 2021. 22. 12. 3941. PMID: 34967575; PMCID: PMC 9080373.
- Rahmani AH, Aldebasi YH, Srikar S, Khan AA, Aly SM. Aloe vera: Potential candidate in health management via modulation of biological activities. Pharmacogn Rev. 2015 Jul- Dec; 9 (18): 120- 6. doi: 10. 4103/ 0973-7847.162118. PMID: 26392709; PMCID: PMC 4557234.
- Gupta VK, Malhotra S. Pharmacological attribute of Aloe vera: Revalidation through experimental and clinical studies. Ayu. 2012 Apr; 33 (2): 193- 6. doi: 10. 4103/ 0974- 8520.105237. PMID: 23559789; PMCID: PMC 3611630.
- Khan MA, Gupta A, Sastry JL, Ahmad S. Hepatoprotective potential of kumaryasava and its concentrate against CCl4-induced hepatic toxicity in Wistar rats. J Pharm Bioallied Sci. 2015 Oct-Dec; 7 (4): 297- 9. doi: 10. 4103/ 0975-7406. 168029. PMID: 26681887; PMCID: PMC 4678989.
- Surjushe A, Vasani R, Saple DG. Aloe vera: a short review. Indian J Dermatol. 2008; 53 (4):163- 6. doi: 10. 4103/ 0019- 5154. 44785. PMID: 19882025; PMCID: PMC 2763764.
- Khan AW, Kotta S, Ansari SH, Sharma RK, Kumar A, Ali J. Formulation development, optimization and evaluation of aloe vera gel for wound healing. Pharmacognosy Mag. 2013 Oct; 9(Suppl 1): S6- S10. doi 10. 4103/ 0973-1296. 117849. PMID: 24143047; PMCID: PMC 3798142.
- Shukla Upadhyay K, Karunagoda K, Sata N, Dei LP. Effect of Kumari Taila Uttar Basti on fallopian tube blockage. Ayu. 2010 Oct; 31 (4): 424- 9. doi: 10. 4103/ 0974- 8520. 82031. PMID: 22048533; PMCID: PMC 3202247.
- Maurya DK, Sharma D. Evaluation of traditional ayurvedic Kadha for prevention and management of the novel Coronavirus (SARS- CoV- 2) using in silico approach. J Biomol Struct Dyn. 2022 Jun; 40 (9): 3949- 3964. doi 10.1080/ 07391102. 2020. 1852119. Epub 2020 Nov 30. PMID: 33251972; PMCID: PMC 7754934.
- Chumbhale, Deshraj & Chaudhari, SR & Upasani, CD. (2014). STANDARDIZATION OF MARKETED KUMARI ASAVA- A POLYHERBAL AYURVEDIC FORMULATION. INTERNATIONAL JOURNAL OF PHARMACEUTICAL, CHEMICAL AND BIOLOGICAL SCIENCES. 4. 681-685.
- Sánchez, Marta & González-Burgos, Elena & Iglesias, Irene & Gómez-Serranillos, Maria. (2020). Pharmacological Update Properties of Aloe Vera and its Major Active Constituents. Molecules (Basel, Switzerland). 25. 10. 3390/ molecules 25061324.
- Jawanjal, Pravin & Cholera, MS & Bedarkar, Prashant & Patgiri, BJ & Harisha, Channappa. (2020). Different diagnostic modalities for the study of Kumari (Aloe vera (l.) burm.) swarasa (Juice) Bhavita Trivanga Bhasma concerning baseline microbial profile. Medical Journal of Dr. D.Y. Patil Vidyapeeth. 13. 498. 10. 4103/ mjdrdypu. mjdrdypu_209_19.
- Elamthuruthy, A & Kothari, Charmy & Khan, Tabassum & Tatke, Pratima & Gabhe, SY. (2005). Standardization of marketed Kumariasava – An Ayurvedic Aloe vera product. Journal of pharmaceutical and biomedical analysis. 37. 937- 41. 10. 1016/ j. jpba. 2004. 11. 044.
- Krunal, A & Doshi, Krunal. (2015). ” KUMARI (Aloe vera Tourn. ex Linn.) ” A MIRACULOUS HERB ON THE EARTH- A CLASSICAL REVIEW. International Journal of Ayurvedic and herbal medicine. 5. 3- 2015. Jawanjal, Pravin & Cholera, MS & Bedarkar, Prashant & Patgiri, BJ. (2019). Stability study of Kumari (Aloe vera [L.] burm.) Swarasa (juice) concerning baseline microbial diagnostic modalities. BLDE University Journal of Health Sciences. 4. 60. 10. 4103/bj’s. bjhs_50_19.
- v. S, Nimmy & Sheba, M. (2021). EXPLORING THE PHARMACO-THERAPEUTIC EFFICACY OF KUMARI (ALOE VERA L.) ON THE REPRODUCTIVE SYSTEM. World Journal of Pharmaceutical Research. 10. 1593. 10. 20959/ wjpr 20214- 20189.
- Dhiman, Sonia & Upadhyaya, Ashwani & Sharma, Navneet & Srivastava, Rashmi & Shukla, Seema. (2012). PA01. 65. Comparative study of kumari swarasa and kanyasara in management of kashtartava. Ancient Science of Life. 32. 115. 10. 4103/ 0257- 7941. 112122.
- TA, Dr & AP, Sole. (2020). Efficacy of Kumari [Alove Vera (L)] on Agnidagdha Vrana (Burn Wound) With Special Reference to Ayurvedic and Modern Aspect: A Review. Scholars International Journal of Traditional and Complementary Medicine. 03. 1- 11. 10. 36348/ sijtcm. 2020. v03i01. 001.
- Pathak, Divya & Sharma, Rajesh. (2017). REVIEW ON ” ALOE VERA-MEDICINAL PLANT “. IJARIIE. 1. 2017- 2395.
- Rout, Kedar & Rout, Om & Mishra, Sagar. (2009). Standardization of Ayurvedic Formulations Containing Aloe vera by Quantification of a Marker Compound. JPC – Journal of Planar Chromatography – Modern TLC. 22. 381- 384. 10. 1556/ JPC. 22. 2009. 5. 13.
- Rajeswari, R. & Manivannan, Umadevi & Rahale, Sharmila & Pushpa, R. & Selvavenkadesh, S. & Kumar, K. & Bhowmik, Debjit. (2012). Aloe vera. Journal of Pharmacognosy and Phytochemistry. 1. 118- 124.
- Gupta, Akhilesh & Rawat, Swati Rawat. (2017). Clinical importance of aloe vera: Review. Research Journal of Topical and Cosmetic Sciences. 8. 30- 39. 10. 5958/ 2321- 5844. 2017. 00004. 8.
- Yadav, Rashmi & Kumar, Sanjeev & Dwivedi, Kamal. (2019). A BRIEF REVIEW OF MEDICINAL PROPERTIES OF KUMARI (Aloe vera Tourn.) FROM KOSHA AND NIGHANTUS.
- Raokhande, Renu. (2020). Therapeutic and nutritional values of Kumari (Aloe Vera)- a review. National Journal of Research in Ayurved Science. 8. 10. 52482/ ayurlog. v8i02. 567.
- Rawat, Swati Rawat & Gupta, Akhilesh. (2017). Clinical importance of aloe vera.
- Gupta, Brij Mohan & Kk, Mueen & Dhawan, Surinder & Gupta, Ritu. (2017). Aloe Vera (Medicinal Plant) Research: A Scientometric Assessment of Global Publications Output during 2007-16. Pharmacognosy Journal. 10. 01- 08. 10. 5530/jp. 2018. 1. 1.
- Sahu, Pankaj & Giri, Deen & Singh, Ritu & Pandey, Priyanka & Gupta, Sharmistha & Shrivastava, Atul & Kumar, Ajay & Pandey, Kapil. (2013). Therapeutic and Medicinal Uses of Aloe vera: A Review. Pharmacology & Pharmacy.
- Qadir, M. (2009). Medicinal and cosmetologically importance of Aloe vera. International Journal of Natural Therapy. 2. 21- 26.
- Lanka, Suseela. (2018). A REVIEW ON ALOE VERA-THE WONDER MEDICINAL PLANT. Journal of Drug Delivery and Therapeutics. 8. 10. 22270/ jddt. V 8i5- s.1962.
- Datta, Animesh & Mandal, Aninda & Teixeira da Silva, Jaime & Saha, Aditi & Sengupta, Sonali & Dubey, Priyanka Kumari & Halder, Sandip. (2012). An updated overview on Aloe Vera (L.) Burm. f. Medicinal and Aromatic Plant Science and Biotechnology (Global Science Books). 6. 1- 11.
- Surjushe, Amar & Vasani, Resham & Saple, D.G. (2008). Aloe vera: A short review. Indian Journal of Dermatology. 53. 163- 6. 10. 4103/ 0019- 5154. 44785.
- Kumar, K & Bhowmik, Debjit & Bhattacharjee, Chiranjib & Biswajit, (2010). Aloe vera: A Potential Herb and it’s Medicinal Importance. 21-29.
References
- Agnivesha, Charaka, Dridhabala. In: Charaka Samhita, ed. Vaidya Jadavaji Trikamji Aacharya., editor. Varanasi: Chaukhamba Sanskrit Sansthan; 2009.
- Sushruta. In: Sushruta Samhita, Sutra Sthana, ed. Vaidya Jadavji Trikamji Acharya., editor. Varanasi: Choukhambha Orientalia; 2005.
- Vagbhata. In: Ashtanga Hrudaya, 9th ed. Anna Moreshwar Kunte, Krishnashastri Navarre, Harishastri, editors. Varanasi: Choukhambha Orientalia; 2005.
- Bhavamishra. In: Bhava Prakasha Nighantu, Guduchyadi Varga 11th ed. part 2. Brahma Shankara Mishra., editor. Varanasi: Choukhambha Bharati Academy; 2009.
- Bhavprakasha, commentary by Bulusu Sitaram, forwarded by K.C.Chunekar
- Sharma PV, Kaideva Nighantu. Aushadhi Varga. Chaukhamba Orientalia, Varanasi; 2006:
- Tripathi I., Raja Nighantu, Parpatadi Varga, Chaukhamba Krishnadas Academy; Varanasi; 2010
- Priya Nighantu by P. V. Sharma, Shatpushpadi Varga Chaukhamba Krishnadas Academy; Varanasi.
- Dr. Gyanendra Pandey, Dravyaguna Vigyana, reprint 2012, Chawkhamba Krishnadas Academy
- Vaidya Manorma, 16/ 101- 102
- K. Niteshwar Dravyaguna Vigyan, reprint 2017.
- Dr. J.L.N. Sastry and Dr. B.S. Sastry, Dravyaguna Vigyana, Chaukhambha Orientalia, Varanasi.
- Chakrapanidatta, Chakradatta with the vaidaya Prabha hindi commentary by indra deva tripathi, chaukambha sanskrita sansthan, varanasi 2nd Edition, 1994.
Ayurveda is an Indian system of medicine that is popular since ancient times. Dr. Gupta’s IAFA® has been conducting research studies to find out different phytoconstituents of herbs and their action in the body. Such knowledge acquired by our experts is used in the preparation of medicines and providing the treatment facilities safely and effectively. IAFA® is the provider of safe and effective treatment for a wide range of diseases, mainly allergic diseases all based on Ayurveda.
Was this Page Helpful?
Read More Articles

Daruharidra (Berberis aristata)
Explore the uses, benefits, and medicinal properties of Daruharidra (Berberis aristata), also…

Haridra (Curcuma longa)
Discover the uses, benefits, and medicinal properties of Haridra (Curcuma longa), also…

Bhumi Amla (Phyllanthus Niruri)
Know the Uses, Benefits and Medicinal Properties of Bhumi Amla (Phyllanthus Niruri).…












